Bone Metastasis: What It Is, How It Affects You, and What Treatments Help
When bone metastasis, the spread of cancer from its original site to the bones. Also known as secondary bone cancer, it doesn’t mean the bone itself is cancerous—it means cancer cells from the breast, prostate, lung, or other organs have traveled and taken root in the bone tissue. This isn’t rare. About 70% of people with advanced breast or prostate cancer develop bone metastases. For lung cancer, it’s close to 30-40%. The bones don’t fight back—they just become a landing zone for aggressive cells that break down bone structure, causing pain, fractures, and sometimes high calcium levels in the blood.
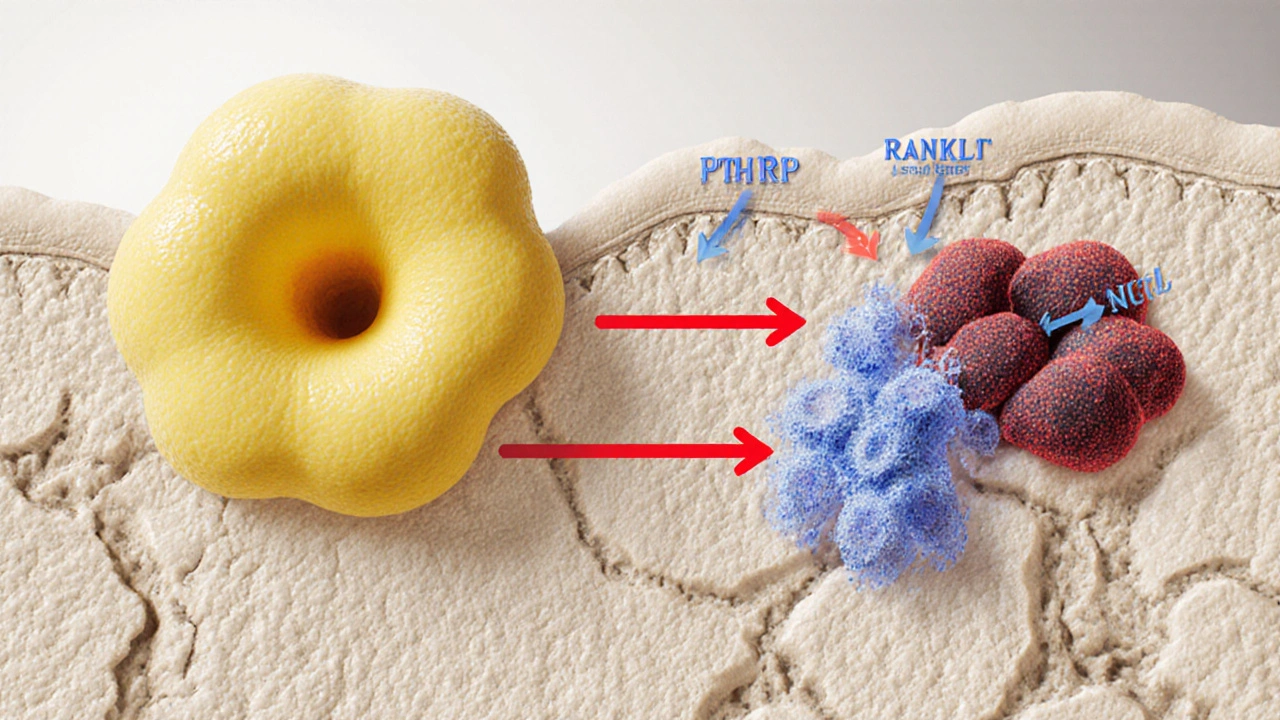
What makes bone metastasis so tricky is that it often shows up late. You might feel a dull ache in your back, hip, or ribs and think it’s just aging or a pulled muscle. But if you’ve had cancer before, that persistent pain could be something more. The cancer cells release chemicals that activate bone-eating cells called osteoclasts. This weakens the bone from the inside, making it fragile. In some cases, even a minor fall or cough can cause a fracture. And when bone breaks down, calcium leaks into the bloodstream, which can lead to fatigue, confusion, or even kidney problems.
There’s no cure for bone metastasis, but there are ways to slow it down and make life more manageable. Treatments like bisphosphonates, drugs that help strengthen bone and reduce fractures in cancer patients are commonly used. Radiation therapy can target painful spots quickly. Newer drugs like denosumab block the cells that destroy bone. And if the original cancer is still active—say, breast or prostate cancer—hormone therapy or chemotherapy may be used to shrink the source. Pain control is just as important. Many patients need strong painkillers, nerve blocks, or even physical therapy to stay mobile.
You’ll also hear about palliative care, a focused approach to improving quality of life for people with serious illness. This isn’t about giving up—it’s about living better. Palliative teams help with pain, nausea, anxiety, and even financial stress. They work alongside your oncologist to make sure you’re not just surviving, but able to sleep, move, and spend time with loved ones.
What you’ll find in the posts below isn’t a textbook. It’s real, practical info from people who’ve been there. You’ll see how capecitabine helps slow bone spread in some cancers, how pain meds like meloxicam are used (and where they fall short), and what alternatives exist when standard treatments don’t work. You’ll find guides on managing side effects, dealing with fatigue, and even how to talk to your doctor when things get overwhelming. This isn’t about hope in the abstract—it’s about what actually works on the ground, day after day.
Learn how tumor growth harms bone health, the mechanisms behind bone metastasis, signs to watch for, and strategies to protect skeletal strength.