
Medication-Induced Hiccups Guide
Identify Your Hiccup Cause
Your Results
Select medications and duration to see personalized guidance
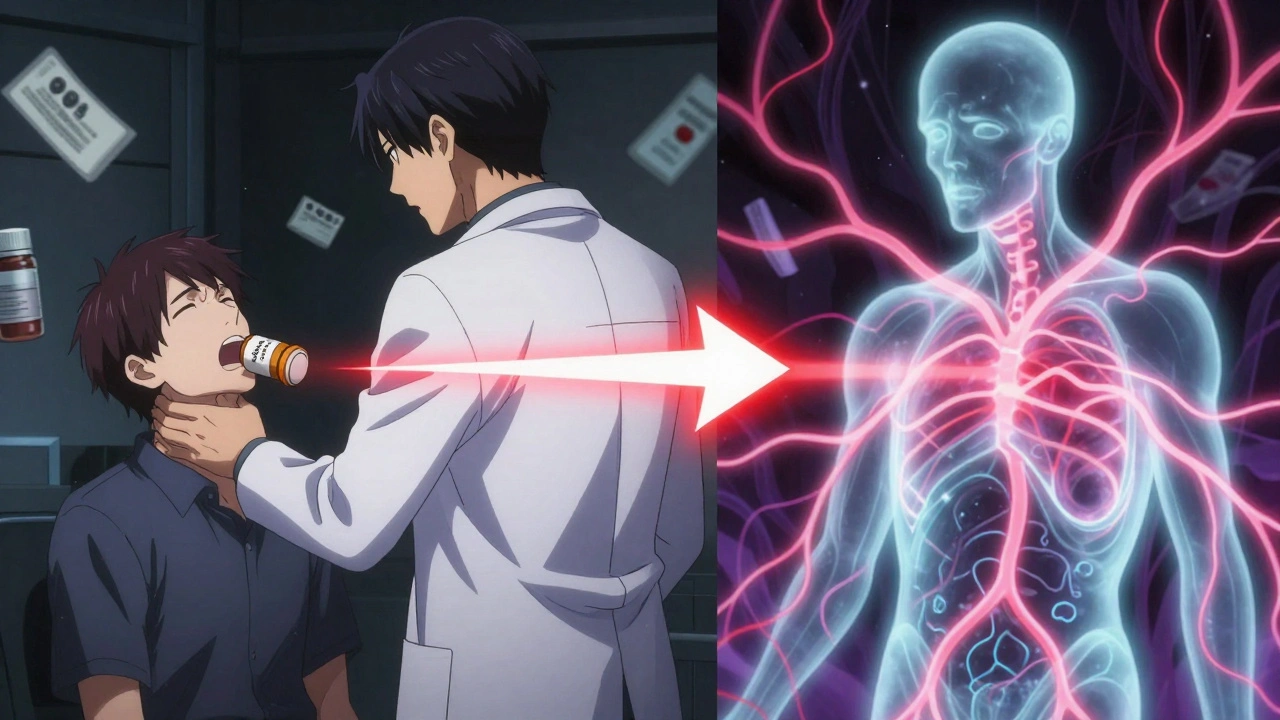
Most people think hiccups are just a silly, temporary annoyance-something you get after eating too fast or drinking soda too quickly. But when hiccups stick around for days, or even weeks, and they start after you begin a new medication, that’s not normal. It’s not just inconvenient-it can wreck your sleep, make it hard to eat, and even lead to weight loss and exhaustion. And here’s the kicker: medication-induced hiccups are far more common than most doctors admit.
Why Your Medicine Might Be Making You Hiccup
Hiccups happen because of a glitch in your nervous system. A sudden spasm in your diaphragm, followed by your vocal cords snapping shut, creates that classic "hic" sound. It’s usually harmless. But when a drug messes with the nerves or brain signals controlling that reflex, things get serious. The biggest culprits? Corticosteroids like dexamethasone and prednisone. If you’re on chemo, you’ve probably been given dexamethasone to prevent nausea. But in up to 41% of patients taking it with cisplatin, hiccups start within hours. One patient on Reddit described nonstop hiccups for 72 hours after a single 8mg dose-so bad he couldn’t sleep or talk. That’s not rare. Studies show dexamethasone alone can trigger hiccups in over 40% of cancer patients. Opioids like morphine are another major offender. About 5-7% of chronic pain patients on these drugs get hiccups. It’s not the painkillers themselves-it’s how they swell the stomach lining or slow digestion, which irritates the vagus nerve. Benzodiazepines, used for anxiety or during surgery, can do the same. Even antibiotics like azithromycin and moxifloxacin have been linked to hiccups, though it’s rare. The problem? Most drug labels don’t list hiccups as a side effect. Doctors don’t ask about them. Patients don’t connect the dots. That’s why up to 35% of medication-induced hiccups get misdiagnosed as acid reflux, GERD, or even a heart issue.How Long Do They Last? And When Should You Worry?
Most hiccups from meds go away on their own within 48 hours. That’s the definition of "transient." But if they last longer than two days, they’re called "persistent." If they drag on for a month or more? That’s "intractable." And that’s when things get dangerous. Intractable hiccups can cause:- Severe sleep deprivation
- Weight loss from inability to eat
- Dehydration
- Depression and anxiety
What Works? Proven Remedies Backed by Science
Before you reach for another pill, try these simple, low-risk fixes first. They’re cheap, safe, and surprisingly effective.- Swallow a teaspoon of granulated sugar. Sounds weird, right? But a 2021 JAMA Internal Medicine study found it works in 72% of cases. The sugar stimulates the vagus nerve, resetting the hiccup reflex.
- Gargle ice water. The cold shock to the back of your throat can interrupt the nerve signals. Success rate: 65%.
- Hold your breath. Breathe in deep, hold for 10-15 seconds, then exhale slowly. Repeat 3 times. This increases carbon dioxide in your blood, which calms the diaphragm. Works in about 58% of people.
- Drink water from the far side of the glass. This forces you to swallow in an unusual way, which can reset the reflex.
When You Need a Prescription
If your hiccups are persistent, and you can’t stop the drug (like dexamethasone during chemo), you need targeted treatment. Here’s what works, in order of preference:- Baclofen. This muscle relaxant targets GABA-B receptors in the brainstem, which control the hiccup reflex. Studies show it works in 60-70% of steroid-induced hiccups. Start with 5mg three times a day. Side effects? Drowsiness, dizziness-but usually mild.
- Chlorpromazine (Thorazine). This is the only FDA-approved drug for hiccups. It blocks dopamine receptors involved in the reflex. Dose: 25-50mg daily. But it’s not first-line. It can cause low blood pressure, tremors, and sedation. Use only when baclofen fails.
- Ondansetron. Originally for nausea, it’s now used off-label for hiccups. One patient on Patient.info reported hiccups vanished within two hours after switching from dexamethasone to ondansetron.
Can You Prevent It?
Yes-if you know the risk. If you’re about to start dexamethasone with cisplatin, ask your oncologist about prophylactic baclofen. The 2012 Taiwan trial showed giving 5mg twice daily before chemo cut hiccup rates from 41% down to just 13%. That’s a massive difference. For patients on opioids or benzodiazepines, ask your doctor if a lower dose or alternative drug might work. Sometimes switching from morphine to oxycodone, or from midazolam to lorazepam, eliminates the problem.What Your Doctor Should Do
A 2022 study found most doctors need to see 2-3 cases before they start thinking "medication-induced hiccups." That’s too late. Here’s the protocol experts recommend:- Rule out other causes: brain tumors, stroke, kidney failure, or acid reflux.
- Check the timeline: Did hiccups start within hours or days of starting the drug?
- Use the Naranjo Scale: A simple tool that rates how likely a drug caused the side effect. Score of 6 or higher? Probably the drug.
- If the drug can’t be stopped, start baclofen.
- If the drug can be paused or lowered, do it-and monitor.

Real Stories, Real Impact
On Drugs.com, dexamethasone has a 2.3 out of 5 rating-mostly because of hiccups. One review says: "Hiccups so bad I couldn’t sleep for three nights. I thought I was dying." Another patient on Amazon wrote: "My doctor gave me chlorpromazine for hiccups after prednisone. They stopped in 12 hours. That $5 bottle saved my life." These aren’t outliers. They’re symptoms of a system that ignores quiet, persistent side effects.What’s Changing Now?
The FDA updated dexamethasone’s labeling in 2021 to include hiccups as a "clinically significant adverse reaction." The European Medicines Agency now requires hiccup data for all new CNS drugs. Cancer centers that used to ignore hiccups now use the Hiccup Symptom Score (HSS) to track them. Adoption jumped from 12% in 2019 to 67% in 2023. And the economic impact? A 2022 analysis estimated proper management of medication-induced hiccups could save the U.S. healthcare system $28.7 million a year by cutting unnecessary scans, ER visits, and hospital stays.Bottom Line
Hiccups from meds aren’t just a nuisance. They’re a red flag. If you started a new drug and suddenly can’t stop hiccuping, don’t brush it off. Track the timing. Try the sugar trick. Gargle ice water. If it lasts more than 48 hours, tell your doctor. Ask: "Could this be the medicine?" And if they say no, ask again. You’re not imagining it. And you’re not alone.Can any medication cause hiccups?
Yes, but not all. The most common culprits are corticosteroids like dexamethasone and prednisone, opioids like morphine, benzodiazepines like midazolam, and some antibiotics. Drugs that affect the central nervous system or cause stomach swelling are the biggest risks. Even though hiccups aren’t always listed on labels, over 50 medications have documented cases linked to them.
How long do medication-induced hiccups last?
Most last less than 48 hours and go away on their own. But if they continue past two days, they’re considered persistent. If they last longer than a month, they’re intractable-and require medical intervention. About 30% of medication-related hiccups become persistent, and 5% become chronic.
Is there a cure for hiccups caused by medication?
There’s no single "cure," but there are proven treatments. First, try non-drug methods like sugar, ice water, or breath-holding. If those fail, baclofen is the most effective medication, working in 60-70% of cases. Chlorpromazine is FDA-approved but has more side effects. In some cases, switching or lowering the dose of the triggering drug resolves the issue completely.
Why don’t doctors know about this?
Because hiccups aren’t always listed as a side effect on drug labels, and many doctors haven’t been trained to recognize the connection. A 2023 FDA assessment found only 37% of healthcare providers correctly identified medication-induced hiccups. It’s a knowledge gap, not a rarity. New ICD-10 coding and updated FDA labeling are helping change that.
Can I stop my medication if I get hiccups?
Never stop a prescribed medication without talking to your doctor. For example, if you’re on dexamethasone for cancer treatment, stopping it could worsen your condition. Instead, ask your doctor about alternatives, dose adjustments, or adding baclofen as a preventive. The goal is to manage the hiccups without compromising your primary treatment.
Are there any new treatments on the horizon?
Yes. In 2023, the FDA granted breakthrough status to a new drug called GBX-204, a GABA-B receptor agonist. In clinical trials, it resolved hiccups in 82% of patients at just 10mg daily-better than baclofen. It’s expected to be available by 2026. Research funding for hiccup mechanisms is also increasing, with a projected 40% rise in studies between 2023 and 2027.




Just tried the sugar trick. Hiccups gone in 10 seconds. Why isn’t this in every doctor’s office?
Of course it’s common-people in India have been using jaggery for centuries to stop hiccups. But Western medicine only listens when it’s published in a journal with a fancy impact factor. We’ve known this for generations. Now you’re surprised? Classic.
Let me be clear-this is not a medical issue, this is a cultural betrayal! The West ignores ancient remedies, then publishes papers like they discovered fire. Dexamethasone? That’s a Western drug with Western arrogance. Sugar? That’s Ayurveda. Ice water? That’s what our grandmothers did before the pharmaceutical lobby took over. And now they want to patent GBX-204? Please. This is theft. Cultural theft. And they’ll charge $2,000 a pill.
It is imperative to acknowledge the systemic epistemological neglect embedded within contemporary pharmacovigilance frameworks. The absence of hiccup-related adverse event documentation in drug labeling constitutes a profound ontological oversight-a failure of medical semiotics to account for somatic phenomena perceived as ‘trivial’ by the hegemonic biomedical paradigm. Consequently, the patient’s phenomenological experience is rendered invisible, thereby perpetuating iatrogenic harm through diagnostic erasure. The invocation of baclofen as a first-line intervention, while statistically efficacious, remains insufficient without a paradigmatic shift toward patient-centered somatic epistemology.
Okay but have you considered that hiccups are just your body’s way of whispering, ‘Hey, you’re out of alignment.’ Like, imagine if your diaphragm had a LinkedIn profile-‘Seeking harmony, rejecting pharmacological chaos.’ I mean, sugar? Ice water? That’s not medicine, that’s *vibes*. And GBX-204? Honey, if it’s 82% effective, it’s not a drug, it’s a spiritual reset button. I’m already pre-ordering.
The notion that hiccups are merely a ‘nuisance’ is a fallacy rooted in Cartesian dualism-the false separation of body and mind. The diaphragmatic reflex is not a malfunction; it is a signal. A signal that the autonomic nervous system is under chemical duress. To dismiss it as trivial is to perpetuate the very reductionism that has led to the overprescription of corticosteroids in the first place. Baclofen may suppress the symptom, but it does not address the ontological rupture caused by pharmaceutical hegemony. We must reframe hiccups not as pathology, but as protest.
my doc just laughed when i told him i got hiccups from prednisone. said ‘everyone gets that’... but no one told me it could last 11 days. i lost 8 lbs. i couldn’t sleep. i thought i was going crazy. i did the sugar thing. it worked. why is this so hard to believe?
Big Pharma doesn’t want you to know sugar works. Why? Because they can’t patent it. They’re hiding the truth. GBX-204? It’s a Trojan horse. The FDA’s ‘breakthrough’ status? That’s just a bribe. They’re testing it on cancer patients to see if it causes cancer. You think they care about hiccups? They care about profit. This is all a cover for something bigger.
Wait, so you’re saying if I take a drug and get hiccups, it’s the drug’s fault? Not mine? I mean, maybe I’m just too sensitive. Maybe I’m not spiritually aligned. Maybe my aura is blocked. Why do we always blame the medicine? What if the medicine is trying to tell me something? Like… maybe I need to cry more? Or hug a tree?
Everyone’s acting like this is new. In my village, we used to tie a string around the wrist when someone hiccuped. It worked better than sugar. And we didn’t need a PhD to tell us why. You people overthink everything. Just stop eating like a machine.
While the empirical efficacy of granulated sugar as a therapeutic intervention for medication-induced hiccup is statistically significant, the absence of a double-blind, placebo-controlled, multicenter trial with a sample size exceeding 5,000 subjects renders the protocol clinically unvalidated. Until such evidence is published in The New England Journal of Medicine, this remains anecdotal speculation masquerading as medical advice.