
When you have inflammatory bowel disease (IBD)-whether it’s Crohn’s disease or ulcerative colitis-and you’re thinking about getting pregnant, the biggest question isn’t just can I get pregnant? It’s can I stay safe-for you and your baby?
For years, women with IBD were told to stop their meds before trying to conceive. Many did-and ended up in the hospital with flare-ups. Others delayed pregnancy out of fear. But the truth today is simpler: uncontrolled IBD is far more dangerous to your pregnancy than the medications that keep it in check.
According to the Helmsley PIANO Global Consensus (2023), women with active IBD at conception are 2.3 times more likely to have a preterm baby, 1.8 times more likely to have a low-birth-weight baby, and 1.6 times more likely to experience stillbirth than those in remission. That’s not a small risk. That’s the kind of risk you can actually prevent.
What Medications Are Safe During Pregnancy?
The good news? Most IBD medications are safe-or at least, much safer than letting your disease run wild.
Aminosalicylates (5-ASAs) like mesalamine and sulfasalazine are the oldest and most studied. Major guidelines from the Crohn’s & Colitis Foundation and ECCO all say: keep taking them. They don’t increase birth defects, miscarriage, or preterm birth. But there’s a catch: not all mesalamine brands are equal.
Some older formulations, like Asacol HD, use a coating called dibutyl phthalate (DBP). Animal studies and human data show DBP can cause genital malformations in male babies at high doses. So if you’re on mesalamine, check your brand. Lialda, Delzicol, Apriso, and Mesalamine ER are DBP-free and safe. Ask your pharmacist. Don’t assume your prescription hasn’t changed.
Sulfasalazine is also safe, but it blocks folate absorption. That’s why your doctor will likely give you a higher dose of folic acid-5 mg daily-starting at least three months before conception. Folate isn’t just for neural tube defects; it helps your baby’s entire development.
Biologics: The New Gold Standard
Biologics like infliximab (Remicade) and adalimumab (Humira) have been used in over 2,000 pregnancies tracked in the PIANO registry. The results? No increase in birth defects. No spike in preterm births. No higher risk of infections in newborns.
These drugs cross the placenta, especially in the third trimester. That’s why some doctors reduce the dose or delay the last injection until week 30-just to lower the amount of drug the baby is exposed to right before birth. But stopping them completely? That’s risky. Flares during pregnancy are harder to treat and more dangerous than a baby having trace amounts of medication.
Vedolizumab (Entyvio) is newer, but data from 103 pregnancies shows no major safety red flags. Babies born to moms on vedolizumab had similar infection rates and no birth defects. One early study showed lower live birth rates-but when researchers removed women who had active disease during pregnancy, that gap disappeared. So again, it’s not the drug. It’s the inflammation.
Ustekinumab (Stelara) is also now well-supported. Over 680 pregnancies in global safety databases show outcomes matching the general population. A 2024 European study of 78 infants found no increased risk of prematurity, low birth weight, or malformations-even when moms got induction doses early in pregnancy.
What to Avoid at All Costs
There are two medications you must stop before trying to conceive: methotrexate and thalidomide.
Methotrexate is a known teratogen. It causes severe birth defects-cleft palate, brain malformations, limb problems-in 17% to 27% of exposed pregnancies. It’s not a risk. It’s a guarantee. You need to stop it at least three months before conception, and your doctor should confirm it’s fully out of your system with blood tests.
Thalidomide? It’s not even on the table. It’s banned in pregnancy for good reason. Even a single dose can cause phocomelia-limbs that are missing or underdeveloped. If you’ve ever taken it for IBD (rare, but possible in refractory cases), you must use two forms of birth control and get regular pregnancy tests.
JAK Inhibitors: Proceed with Caution
Drugs like tofacitinib (Xeljanz) and upadacitinib (Rinvoq) are newer, effective, and popular. But they work by blocking the JAK-STAT pathway, which plays a role in early embryonic development.
So far, small studies (11 pregnancies for tofacitinib, 98 for upadacitinib) haven’t shown clear harm. But experts still recommend stopping them at least 4-6 weeks before conception. Why? Because the data is limited. And when it comes to pregnancy, caution isn’t fear-it’s responsibility.
If you’re on a JAK inhibitor and want to get pregnant, talk to your gastroenterologist now. Switch to a biologic or 5-ASA first. Don’t wait until you miss a period.
What About Steroids?
Corticosteroids like prednisone are sometimes used to treat flares. But they’re not ideal during pregnancy.
First-trimester use is linked to a 1.4 to 2.3 times higher risk of cleft lip or palate. That’s why guidelines say: use steroids only if absolutely necessary-and try to taper off before conception. If you’re on long-term steroids, work with your doctor to switch to a safer maintenance drug before you start trying.
Immunomodulators: Azathioprine and 6-MP
These drugs-azathioprine (Imuran) and mercaptopurine (6-MP)-have been used safely in pregnancy for decades. Studies show no increase in birth defects, stillbirth, or childhood cancers.
They’re often used when biologics aren’t an option or as add-ons. You’ll need regular blood tests to monitor your white blood cell count, but they’re generally considered low-risk. Most experts say: keep taking them. Stopping increases your flare risk-and that’s the real danger.
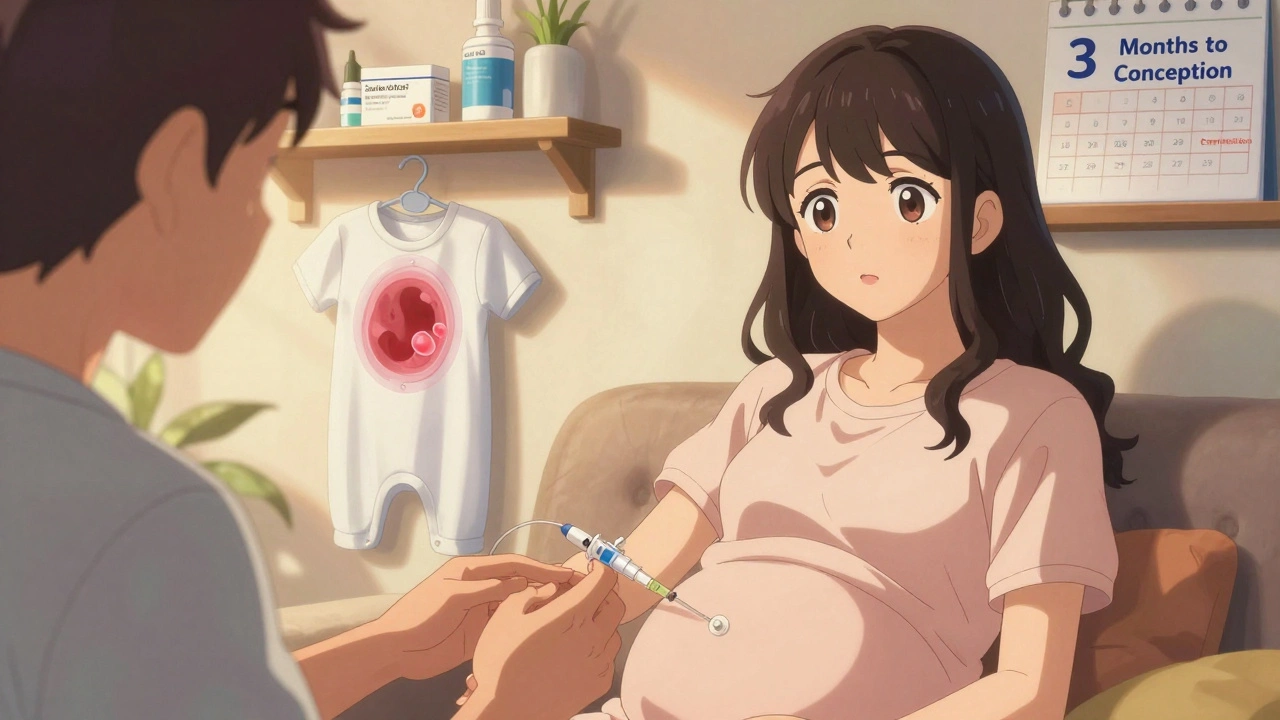
Planning Ahead: The 3-Month Rule
The best time to optimize your IBD treatment for pregnancy? At least three months before you start trying.
Why? Because it takes time for your body to adjust. If you’re switching from methotrexate to a biologic, you need those three months to clear the old drug and let the new one stabilize your disease. If you’re on a JAK inhibitor, you need time to transition safely.
Also, aim for clinical and endoscopic remission-not just feeling better. That means your colon looks healed on a scope, not just that your diarrhea has improved. Endoscopic remission cuts your risk of complications by half.
Work with both your gastroenterologist and your OB-GYN. Ideally, they should talk to each other. Many clinics now have IBD pregnancy clinics with coordinated care. Ask if yours does.
What Happens After Baby Is Born?
Most IBD medications are safe while breastfeeding. Infliximab, adalimumab, vedolizumab, ustekinumab, azathioprine, and 5-ASAs all pass into breast milk in tiny, harmless amounts. The American Academy of Pediatrics considers them compatible with breastfeeding.
Even if your baby was exposed to anti-TNFs in the womb, they can still get all routine vaccines-including live ones like MMR and varicella. The 2024 ECCO guidelines confirm this. No need to delay.
Just watch for signs of infection in the first few months. Babies exposed to biologics may have slightly lower immune responses in the first 6 months, but that’s normal. Keep up with checkups.
The Bottom Line
Here’s what you need to remember:
- Don’t stop your meds without talking to your doctor. Flares are dangerous.
- Switch to DBP-free mesalamine if you’re on Asacol HD or similar.
- Take 5 mg of folic acid daily if you’re on sulfasalazine.
- Avoid methotrexate and thalidomide completely.
- Stop JAK inhibitors 4-6 weeks before conception.
- Plan your pregnancy at least 3 months ahead.
- Get your disease under control-endoscopically, not just symptomatically.
- Continue your meds through delivery and breastfeeding unless your doctor says otherwise.
Women with IBD can-and do-have healthy pregnancies. The key isn’t avoiding medication. It’s choosing the right ones, at the right time, with the right team.
You’re not a risk. You’re a patient with a plan. And with the right care, your baby will be just fine.
Can I get pregnant if I have IBD?
Yes, absolutely. Most women with IBD can conceive without difficulty. The bigger concern isn’t fertility-it’s whether your disease is under control. Active IBD can make pregnancy riskier, so aim for remission before trying to conceive. Work with your gastroenterologist to optimize your treatment plan at least 3-6 months before you start.
Are biologics safe during pregnancy?
Yes. Anti-TNF drugs like infliximab and adalimumab, as well as vedolizumab and ustekinumab, have been studied in thousands of pregnancies. No increased risk of birth defects, miscarriage, or stillbirth has been found. These medications are now considered first-line options for pregnant women with moderate to severe IBD. Some doctors adjust the timing of doses in the third trimester to reduce infant exposure, but stopping them entirely increases the risk of a flare.
Is mesalamine safe during pregnancy?
Yes-but only if it’s a DBP-free formulation. Brands like Lialda, Delzicol, Apriso, and generic mesalamine are safe. Avoid Asacol HD and other versions with dibutyl phthalate (DBP) coating, which has been linked to genital malformations in male infants. Always check the label or ask your pharmacist to confirm your prescription is safe.
Should I stop my IBD meds if I’m breastfeeding?
No. Most IBD medications, including biologics, 5-ASAs, azathioprine, and 6-MP, are considered safe during breastfeeding. Only tiny amounts pass into breast milk, and studies show no harm to infants. The American Academy of Pediatrics supports continuing these medications while nursing. The benefits of breastfeeding and disease control far outweigh any theoretical risks.
Can I have a normal delivery with IBD?
Yes. IBD itself doesn’t require a C-section. Most women with IBD can deliver vaginally unless there’s a separate medical reason, like a perianal fistula or prior pelvic surgery. Your obstetrician will monitor you closely, but your IBD medications won’t interfere with labor or delivery. In fact, continuing your meds through delivery helps prevent postpartum flares.
What if my IBD flares during pregnancy?
Don’t panic. Flares can be treated safely during pregnancy. Biologics and 5-ASAs are still the first-line options. Steroids may be used short-term if needed, but they’re avoided in the first trimester due to cleft palate risk. The goal is to get you back into remission as quickly as possible. Untreated flares are far more dangerous to your baby than the medications used to treat them.
Is it safe to get vaccinated while pregnant with IBD?
Yes. In fact, it’s recommended. The flu shot, Tdap, and COVID-19 vaccines are all safe during pregnancy and protect both you and your baby. Even if you’re on biologics, you can still get all routine vaccines-including live ones like MMR and varicella after birth. The 2024 ECCO guidelines confirm that IBD medications don’t interfere with vaccine safety or effectiveness.
How do I know if my IBD is truly in remission?
Feeling better isn’t enough. True remission means your colon looks healed on a colonoscopy (endoscopic remission), not just that your symptoms have improved. Studies show that only endoscopic remission reduces the risk of pregnancy complications. Ask your gastroenterologist for a scope before you start trying to conceive. If you’re not in endoscopic remission, your treatment plan may need adjustment.



So let me get this straight-your baby’s gonna be fine if you’re on biologics, but if you skip a dose because you’re scared? Congrats, you just turned your womb into a warzone. IBD flares don’t care about your fears. They just show up with a megaphone and a C-section ticket.
I was on Asacol HD when I got pregnant and had no idea about DBP until my OB asked if my med had a weird coating. Thank god I switched to Lialda before week 8. That tiny detail saved my son’s genital development. Always check the label, ladies. Your pharmacist is your secret weapon.
This is the kind of post that gives hope to people who’ve been told for years to ‘wait until you’re cured.’ You’re not broken. You’re not a risk. You’re a person with a medical condition that’s finally being understood. Thank you for writing this.
Ah yes, the classic ‘biologics are safe’ narrative. Convenient how the pharma-funded studies never mention long-term neurodevelopmental outcomes in children exposed in utero. 😏 I’ve seen kids on anti-TNFs who can’t focus in school. Coincidence? Or just the tip of the iceberg?
They say ‘safe’ but never say what ‘safe’ means. Is it safe like ‘your phone charger is safe’ or safe like ‘this banana hasn’t been irradiated’? Also, why is no one talking about the fact that biologics suppress your immune system? What if your baby gets a cold and can’t fight it? Hmm?
I just want to say: if you’re reading this and you’re scared-you’re not alone. I had a flare at 22 weeks. I was terrified. But I kept my Humira. My daughter is now 3, healthy, and loves tacos. You’ve got this. And yes, you can still breastfeed. Your milk is magic.
The real tragedy? Women still get told to stop meds because ‘it’s better to be safe.’ But ‘safe’ is a lie. The real danger is being ignored by doctors who still think IBD is ‘just a gut thing.’ This post? It’s a middle finger to outdated medicine. 🖕
i was on 6-MP when i got preg and my doc said its fine but i was so scared. turns out my daughter is 2 now and she’s a tiny ninja with zero health issues. just keep doing what your docs say. and take the folic acid. it’s not optional.
I’m from India, and here, most doctors still tell women to stop everything. I had to fly to the U.S. for a second opinion. This article? It’s the reason I’m holding my 6-month-old right now. Thank you.
The data is compelling. However, longitudinal studies beyond age five remain limited. Caution is warranted.
I read this while holding my 10-month-old who was born while I was on Humira. I cried. Not because I was scared-but because I finally felt seen. For years I thought I was selfish for wanting a baby. Turns out, staying on my meds was the most selfless thing I ever did. 🤍
okay so i just found out my mesalamine has dbp and i’m 10 weeks pregnant and i think i’m gonna throw up i didn’t even know what dbp was like??? can i just switch today??? help??? 😭
I’ve been a GI nurse for 18 years. I’ve seen women stop their meds and end up in ICU at 32 weeks. I’ve seen babies born healthy because mom kept her biologic. The science is clear. Trust it. You’re not being reckless. You’re being responsible.
The fact that this information isn’t standard in OB-GYN training is a systemic failure. Every prenatal clinic should have a handout like this. If you’re a provider reading this: share it. Don’t assume your patient knows.
You are not broken. You are not a burden. You are not too risky to be a mom. You are a warrior with a treatment plan. And your baby? They’re going to be just fine-because you fought for them before they even took their first breath. Keep going. You’ve got this.