
Opioid-Antidepressant Interaction Checker
Check Your Medication Combination
This tool identifies potential interactions between opioids and antidepressants that could lead to serotonin syndrome.
Every year, millions of people take opioids for pain and antidepressants for mood - often without realizing they could be mixing two drugs that, together, can trigger a life-threatening reaction. This isn’t theoretical. It’s happening in clinics, emergency rooms, and homes across the U.S. Right now. The culprit? Opioid-serotonin syndrome, a dangerous interaction that’s more common than most doctors admit.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t just a side effect. It’s a medical emergency. It happens when your brain gets flooded with too much serotonin - a chemical that helps regulate mood, sleep, and pain. Too much, and your body goes into overdrive. You might start sweating uncontrollably, your muscles tighten up like steel cables, your heart races, and your body temperature spikes to dangerous levels. In severe cases, you can slip into a coma or die.
This isn’t rare. Between 2018 and 2023, opioid-antidepressant combinations accounted for over a third of all serotonin syndrome cases admitted to U.S. toxicology units. And it’s not just prescription drugs. Over-the-counter cough syrups containing dextromethorphan have caused fatal reactions when mixed with SSRIs like sertraline or fluoxetine. Three deaths in one year came from people taking just 30mg of dextromethorphan - the amount in a single dose of many cough medicines.
Not All Opioids Are Created Equal
Here’s the thing: not every opioid carries the same risk. Some are basically safe. Others? They’re ticking time bombs when combined with antidepressants.
High-risk opioids - the ones you should avoid completely if you’re on an SSRI, SNRI, or MAOI - include:
- Tramadol - This one’s a big one. It doesn’t just relieve pain. It blocks serotonin reuptake, just like an antidepressant. Studies show tramadol increases serotonin syndrome risk by nearly 7 times when taken with SSRIs. In clinical reports, it’s involved in nearly half of all opioid-related serotonin syndrome cases.
- Meperidine (pethidine) - Used mostly in hospitals, this opioid is especially dangerous. It’s been linked to over 20% of documented cases. Many doctors don’t even realize it’s a risk.
- Dextromethorphan - Found in cough syrups like Robitussin DM or Delsym. People think it’s harmless. It’s not. It inhibits serotonin reuptake just like tramadol. And because it’s sold over the counter, patients don’t tell their doctors they’re taking it.
Medium-risk opioids - use with extreme caution:
- Methadone - Even though it doesn’t strongly block serotonin reuptake, it can still trigger serotonin syndrome, especially in people on multiple medications. Its long half-life means it builds up, and interactions with SSRIs can raise its levels by 50%.
- Fentanyl - Usually safe at low doses. But during surgery or with high doses (over 100mcg/kg), it starts activating serotonin receptors directly. Anesthesiologists now warn about this.
Low-risk opioids - these are your best options if you need pain relief and are on antidepressants:
- Morphine - No significant serotonin activity. Safe to use.
- Oxycodone - Minimal effect on serotonin. No proven link to serotonin syndrome in clinical studies.
- Hydromorphone - Like morphine, it doesn’t interfere with serotonin pathways.
- Codeine - Risk is very low, but not zero. One case report showed serotonin syndrome after codeine was combined with venlafaxine and a migraine drug. Still, it’s the safest of the opioids in this context.
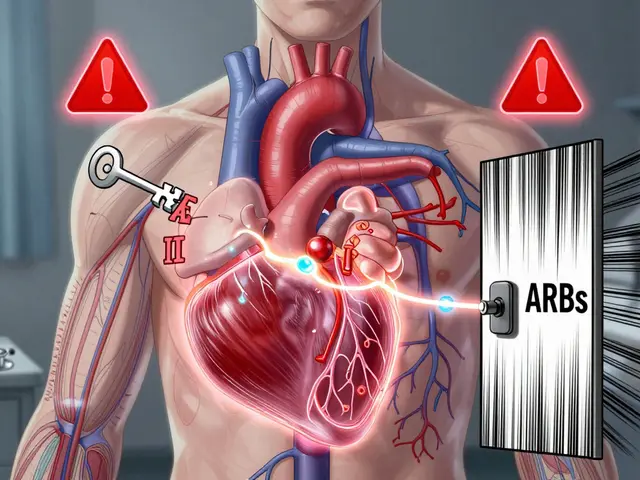
Why This Interaction Happens
It’s not just one mechanism. It’s a perfect storm.
Some opioids - like tramadol - block the serotonin transporter (SERT). That’s the same protein SSRIs target. So when you take both, serotonin piles up in your brain because nothing’s cleaning it up.
Others - like fentanyl and meperidine - directly activate serotonin receptors (5-HT2A), even if they don’t block reuptake. It’s like turning up the volume on a speaker that’s already blasting.
Then there’s the metabolism problem. SSRIs like fluoxetine and paroxetine block the liver enzyme CYP2D6. That enzyme breaks down tramadol into its active painkiller form. So instead of getting pain relief, you get more of the parent drug - which is a serotonin booster. You’re not just adding two drugs. You’re accidentally doubling the serotonin effect.
Real Cases, Real Consequences
A 42-year-old woman in Minnesota started tramadol for back pain while already taking venlafaxine for depression. Within two days, she was admitted to the ICU with a fever of 104.2°F, rigid muscles, and confusion. She didn’t have a history of mental illness - just two common prescriptions. She survived, but barely.
In another case, a 68-year-old man took a daily dose of dextromethorphan for his chronic cough. He was on sertraline for anxiety. He started feeling restless, then developed tremors. Within 12 hours, he was hallucinating and his body temperature hit 105°F. He died before emergency responders arrived.
These aren’t outliers. Between 2015 and 2021, New Zealand’s drug safety agency recorded 41 confirmed cases of opioid-related serotonin syndrome. Tramadol was behind more than half. Dextromethorphan was responsible for 11. And in 3 of those cases, the person was taking the cough medicine at the recommended dose.
What Should You Do?
If you’re on an antidepressant and need pain relief:
- Stop using tramadol, meperidine, and dextromethorphan. These are not safe. Even if your doctor says they’re fine, ask for alternatives.
- Ask for morphine, oxycodone, or hydromorphone. These are effective for pain and don’t raise serotonin levels.
- Check every OTC medicine. Read labels. Dextromethorphan is in more than 150 cough and cold products. Look for "DM" on the bottle.
- Don’t assume your doctor knows. Many physicians still think only MAOIs and SSRIs cause serotonin syndrome. They don’t realize opioids can trigger it too.
- Know the warning signs. Muscle rigidity, high fever, fast heart rate, confusion, agitation, shivering, diarrhea - if you have two or more of these after starting a new pain med, seek help immediately.

What Doctors Should Be Doing
Guidelines from the American Pain Society and the American Society of Anesthesiologists are clear: avoid tramadol and meperidine in patients on serotonergic drugs. Use morphine or oxycodone instead.
But here’s the problem: most doctors don’t screen for this. A 2023 study found that 68% of primary care physicians didn’t ask patients about OTC cough medicines before prescribing opioids. And 42% didn’t know tramadol was a serotonin risk.
Pharmacies are starting to catch up. Some now flag tramadol-SSRI combinations with a red alert in their systems. The FDA added a Black Box Warning to tramadol in January 2023. The European Medicines Agency did the same in 2022. But that doesn’t help if the patient doesn’t know to ask.
The Bigger Picture
Tramadol use in the U.S. has dropped 18% since 2020 - partly because of these warnings. That’s good. It means fewer cases. But dextromethorphan sales are still at 28 million units per year. People don’t think of it as a drug. They think it’s just for coughs.
And genetic factors are now being studied. Some people have a version of the serotonin transporter gene that makes them extra sensitive. Even a small dose of tramadol can push them over the edge.
This isn’t about fear. It’s about awareness. You don’t have to stop pain treatment. You don’t have to stop your antidepressant. You just need to know which combinations are dangerous - and which are safe.
If you’re taking any of these drugs, talk to your doctor. Bring your pill bottles. Ask: "Could this cause serotonin syndrome?" If they hesitate, ask for a pharmacist’s opinion. Or go to a pain specialist. Your life might depend on it.
Can you get serotonin syndrome from just one opioid?
Yes, but only with certain opioids. Tramadol, meperidine, and dextromethorphan can cause serotonin syndrome on their own, especially at high doses. Most other opioids like morphine or oxycodone don’t cause it alone. The real danger comes when you combine them with antidepressants or other serotonergic drugs.
Is serotonin syndrome the same as an opioid overdose?
No. An opioid overdose causes slow breathing, pinpoint pupils, and unconsciousness. Serotonin syndrome causes high fever, muscle rigidity, rapid heart rate, and agitation. They’re opposite in presentation. But both are emergencies. Confusing them can delay the right treatment.
How long after starting a new drug does serotonin syndrome appear?
Usually within 24 to 48 hours, but it can happen as fast as a few hours after taking the first dose. In some cases, it builds slowly over a few days. If you start a new opioid or increase your antidepressant dose, watch for symptoms closely for the first week.
Can I still take antidepressants if I need opioids for pain?
Yes, absolutely. You don’t have to stop your antidepressant. Just avoid high-risk opioids like tramadol and meperidine. Use morphine, oxycodone, or hydromorphone instead. Many patients manage chronic pain and depression safely for years with this approach.
What should I do if I think I have serotonin syndrome?
Stop taking all medications immediately and go to the nearest emergency room. Don’t wait. Bring a list of everything you’ve taken in the last 48 hours - including supplements and OTC cough medicine. Treatment is supportive: cooling, IV fluids, and sometimes cyproheptadine, a serotonin blocker. Early treatment saves lives.
Are there any safe cough medicines if I’m on an SSRI?
Yes. Avoid anything with dextromethorphan. Instead, use guaifenesin (Mucinex) for congestion, or try honey and lemon for cough relief. For nasal symptoms, pseudoephedrine or saline sprays are safe. Always check with your pharmacist before taking any OTC product.



bro i took tramadol with zoloft for a week and felt like my brain was melting but i thought it was just anxiety lmao RIP my sanity
this is so important!! i had no idea cough syrup could kill you 😭 please share this with everyone you know!!
so we're just supposed to trust doctors who don't even know what tramadol does? 🤡 the system is a glitch in the matrix.
The clinical data presented here is compelling and warrants immediate public health attention. The confluence of pharmacokinetic interference and insufficient provider education represents a systemic failure in medication safety protocols.
i lost my cousin to this. they gave him tramadol after surgery. he was on cymbalta. no one warned him. no one.
This is clearly a Big Pharma orchestrated distraction. Why do you think the FDA only issued a black box warning after the 2022 European ruling? The same entities that pushed opioids now push fear of serotonin syndrome to sell 'safer' alternatives. The real danger? Compliance. Control. Surveillance. Check your labels... and your mind.
bro just use ibuprofen 🤦♂️ why are we even talking about this? opioids are for addicts anyway. and dextromethorphan? it's just cough syrup 😂 🤡
I’ve been on sertraline for 8 years, and my doctor just switched me to oxycodone for my sciatica-AND I’M STILL ALIVE!!! 😭🙏 Thank you for this post-I printed it and gave it to my entire family. Don’t be afraid to ask questions-your life is worth more than their 10-minute appointment!