Managing medication for a chronic condition isn’t just about popping pills every day. It’s about staying alive, avoiding hospital visits, and keeping your life as normal as possible. But here’s the hard truth: medication safety for long-term use is one of the most overlooked parts of chronic disease care. People with diabetes, high blood pressure, heart failure, or arthritis often take five, six, or even ten different drugs every day. And that’s where things start to go wrong.
Why Long-Term Medication Use Is Riskier Than You Think
When you’re first diagnosed with a chronic illness, your doctor gives you a script and says, ‘Take this daily.’ It feels simple. But over months and years, prescriptions pile up. You see a cardiologist, a rheumatologist, a neurologist-each adds their own meds. No one steps back to look at the whole picture.
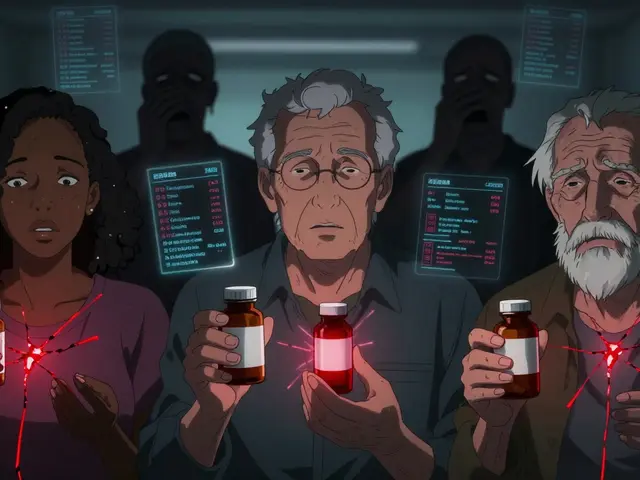
That’s called polypharmacy. And it’s dangerous. Studies show that people taking five or more medications daily are far more likely to experience side effects, falls, confusion, and even early death. The risk isn’t just from one bad drug-it’s from how those drugs interact. For example, mixing aspirin and diclofenac can cause serious stomach bleeding. Taking opioids long-term without monitoring increases overdose risk, even if you’re not addicted.
The Centers for Disease Control found that medication non-adherence contributes to about 125,000 deaths in the U.S. every year. That’s more than car accidents. Most of those deaths are preventable.
The 7 Rights of Safe Medication Use (And How to Use Them)
Healthcare professionals use the ‘7 Rights’ to avoid errors. You should too. These aren’t just for nurses-they’re your personal safety checklist.
- Right patient: Make sure the meds are yours. Never take someone else’s pills, even if they have the same condition.
- Right drug: Know the name of every pill. Don’t rely on color or shape. Ask for the generic name and brand name.
- Right dose: Is it 5 mg or 50 mg? A typo can kill. Always double-check the label.
- Right route: Is it swallowed, injected, or applied to the skin? Taking a patch orally is dangerous.
- Right time: Some meds need to be taken with food. Others must be empty stomach. Timing affects how well they work.
- Right documentation: Keep a written list of every medication-name, dose, frequency, reason, and prescribing doctor. Update it every time something changes.
- Right response: Are you feeling worse? Dizzy? Nauseous? Swollen? Report it immediately. Don’t assume it’s ‘just part of aging.’
Write this list down. Keep it in your wallet. Show it to every doctor, pharmacist, and ER nurse. It’s your best defense against mistakes.
How to Avoid Medication Errors at Home
Most errors happen at home-not in hospitals. Here’s what actually works:
- Use a pill organizer: Not just the cheap plastic kind. Get one with alarms or one that locks. Some even text you when it’s time to take a pill.
- Don’t mix meds in one container: Putting all your pills in a single jar is a recipe for disaster. You’ll forget what’s what.
- Store meds properly: Heat, moisture, and light ruin pills. Don’t keep them in the bathroom cabinet. A cool, dry drawer is better.
- Check expiration dates: Old antibiotics don’t just lose power-they can turn toxic.
- Never skip doses to save money: If you can’t afford your meds, tell your doctor. There are patient assistance programs. Skipping doses causes more harm than cost.
One woman with heart failure skipped her diuretic for weeks because she couldn’t afford it. She ended up in the ER with fluid in her lungs. Her doctor later got her the drug for free through a nonprofit. She didn’t need to suffer.
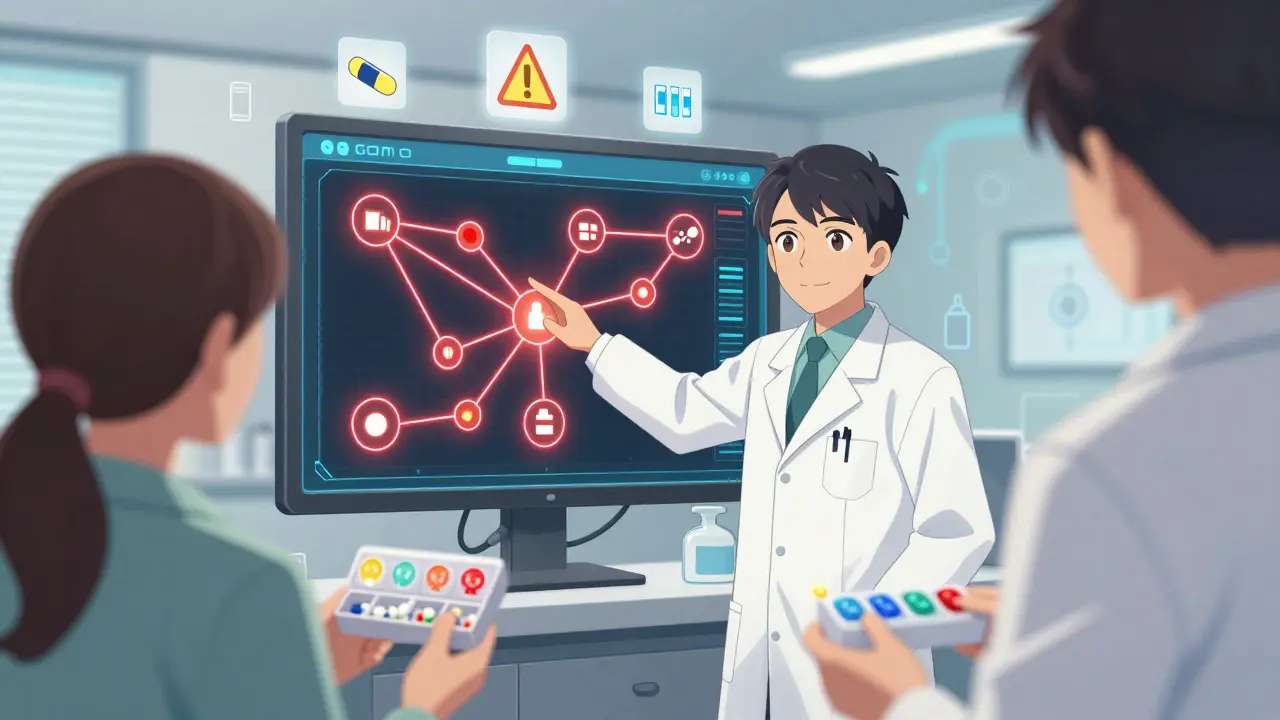
Medication Reviews: Your Secret Weapon
Most people don’t realize they need a full medication review-at least once a year. That means sitting down with your primary care doctor (not a specialist) and going over every single pill, supplement, and over-the-counter drug you take.
The American Geriatrics Society says: Don’t prescribe a new medication without reviewing the whole regimen. That applies to you too. Ask your doctor:
- ‘Is this still necessary?’
- ‘Can any of these be stopped?’
- ‘Are any of these interacting with each other?’
- ‘Is there a cheaper or safer alternative?’
One study found that when pharmacists led these reviews, patients were 89% more likely to stick to their meds. That’s not magic-it’s just someone paying attention.
Technology Can Help-If You Use It Right
You don’t need fancy gadgets. But simple tech tools make a huge difference:
- Pharmacy apps: Many pharmacies send text reminders when your refill is ready. Turn them on.
- Electronic health records: Ask if your doctor uses one. It helps prevent duplicate prescriptions.
- Barcode systems: If you’re in a hospital, ask if they scan your wristband before giving you meds. They should.
- Smart pill dispensers: Devices like Hero or MedMinder dispense pills at the right time and alert you-or your family-if you miss a dose.
These aren’t luxuries. For someone with memory issues or mobility problems, they’re lifesavers.
When to Speak Up-Even If You’re Scared
Doctors are busy. Nurses are stretched thin. You’re the only one who knows how you feel every day.
If you’re experiencing:
- Unexplained dizziness or confusion
- Sudden weight gain or swelling
- Stomach pain, black stools, or vomiting
- Changes in mood, sleep, or energy
-say something. Don’t wait. Don’t think it’s ‘normal.’ It’s not. These could be signs of drug interactions, organ damage, or overdose.
One man took a blood pressure med and a muscle relaxer together. He didn’t realize they both lowered his blood pressure. He passed out while showering, broke his hip, and ended up in rehab for months. He didn’t tell his doctor about the muscle relaxer because he thought it was ‘just for pain.’
What to Do If You’re Overwhelmed
If you’re taking more than five medications, feeling confused, or scared you’re making a mistake, here’s your action plan:
- Get a written list of every medication you take-including vitamins, supplements, and OTC drugs.
- Call your primary care doctor and ask for a medication review appointment.
- Ask if a pharmacist can help you sort your pills and explain what each one does.
- Set up reminders on your phone or use a pill box with alerts.
- Bring a family member or friend to your next appointment. Two ears are better than one.
Don’t wait until something goes wrong. Start today.
Final Thought: Safety Isn’t Optional
Chronic illness doesn’t mean giving up control. It means taking smarter control. Medication safety isn’t about being perfect. It’s about being aware. It’s about asking questions. It’s about knowing your own body well enough to spot when something’s off.
The goal isn’t just to survive. It’s to live-without fear, without hospital stays, without unnecessary side effects. You can do that. But only if you treat your meds like the powerful tools they are-not like background noise.
How many medications is too many for someone with a chronic condition?
Taking five or more medications daily is considered polypharmacy, which significantly increases the risk of side effects, falls, confusion, and hospitalization. While some patients need multiple drugs, each one should be regularly reviewed to ensure it’s still necessary. If you’re on five or more, ask your doctor for a full medication review at least once a year.
Can I stop a medication if I feel better?
Never stop a prescribed medication just because you feel better-especially for chronic conditions like high blood pressure, diabetes, or heart failure. These conditions often have no symptoms when controlled. Stopping meds can cause your condition to rebound dangerously. Always talk to your doctor before making any changes.
What should I do if I miss a dose?
It depends on the medication. For most, if you miss a dose and remember within a few hours, take it right away. If it’s almost time for the next dose, skip the missed one and continue as scheduled. Never double up unless your doctor says so. Check the label or call your pharmacist for specific instructions.
How can I save money on long-term meds without risking my health?
Ask your doctor about generic versions-they’re just as effective and often 80% cheaper. Many drug manufacturers offer patient assistance programs. Pharmacies like Walmart and CVS have $4 generic lists. Don’t skip doses to save money-talk to your provider instead. There are always safer options.
Are over-the-counter drugs safe to take with prescription meds?
Not always. Common OTC drugs like ibuprofen, antacids, sleep aids, and cold medicines can interact dangerously with prescription drugs. For example, ibuprofen can raise blood pressure and damage kidneys when taken with certain heart or kidney meds. Always tell your doctor or pharmacist about every OTC product you use-even if you think it’s harmless.
Why do I need a medication list if my doctor has my records?
Doctors don’t always have access to your full list, especially in emergencies or when seeing specialists. A personal, up-to-date list ensures everyone treating you has the same information. It’s your safety net. Studies show 67% of medication errors happen because of incomplete or missing medication histories during care transitions.



yo so i been takin 7 meds for my diabetes and bp and sometimes i just stare at the pillbox like it’s a riddle from hell 😅
generic names? yeah i know em but half the time the pharmacist says ‘oh this one’s for cholesterol’ and i’m like… wait is this the blue one or the white one??
also i use a pill organizer with alarms but it beeps at 3am and my dog starts barkin like the apocalypse is here. worth it tho.
ps: i asked my doc if i could drop the fish oil and he laughed. said ‘sarthak, if you stop that, your arteries might start throwin a rave.’
Living in the US, I’ve seen this play out way too many times. Elderly folks on 10+ meds, no one coordinating, pharmacy just refillin’ like it’s a vending machine.
My aunt took lisinopril, metformin, and ibuprofen daily for years. One day she passed out in the grocery store. Turns out the combo dropped her BP so low her kidneys almost shut down.
She didn’t even know ibuprofen was risky with her meds. The pharmacist? Didn’t ask. The doctor? Too busy.
Now she has a med review every 6 months. She’s alive. And she still calls me to ask if her green pill is the ‘blood’ one or the ‘sugar’ one.
Knowledge ain’t power unless you use it.
OMG YES 😭 I’m on 8 meds and my pharmacist gave me a SMART pill dispenser that texts my daughter if I miss a dose. She’s 19 and thinks it’s hilarious but I swear, it saved my life last winter when I forgot my heart med and got dizzy in the shower. 🚿💥
Also, I keep my meds in the kitchen drawer now. No more bathroom cabinet! Moisture = bad. I learned that the hard way when my thyroid pills turned into chalk.
PS: I told my doc I don’t need the sleep aid anymore. He said ‘cool, let’s try weaning.’ I said ‘cool, let’s try NOT dying.’ 😎
Oh wow, a whole article about not dying from your own prescriptions? Groundbreaking.
Meanwhile, my cousin took his dad’s blood thinner because ‘it looked like the blue one’ and ended up in the ER with a brain bleed. Dad didn’t even know he was taking it.
So yeah, the 7 Rights? Cute. But the real problem? Doctors don’t talk to each other. Pharmacies don’t care. And patients? We’re just meat sacks with a stack of pills.
Next time your doc prescribes something, ask ‘if I die tomorrow, will anyone know why?’
As a clinical pharmacist with 18 years in geriatric care, polypharmacy is the silent epidemic. The average elderly patient on 5+ meds has a 30% chance of an adverse drug reaction annually.
Drug interactions aren’t theoretical-they’re metabolic. CYP450 enzyme inhibition, renal clearance overlap, QT prolongation cascades-these aren’t buzzwords, they’re death sentences in slow motion.
And yes, the pill organizer with alarms? Non-negotiable. But even better? A structured Medication Therapy Management (MTM) session with a board-certified pharmacist. 89% adherence boost? That’s not anecdotal. That’s JAMA data.
Also: never, ever use a pill splitter without consulting a pharmacist. Dose variability can be ±40% in split tablets.
Medication isn’t just chemistry-it’s identity. For many, each pill is a reminder: ‘I am sick.’ And yet we treat them like objects to be managed, not experiences to be understood.
What if we stopped asking ‘are you taking your meds?’ and started asking ‘how do these pills make you feel about yourself?’
I’ve sat with people who skipped insulin because they hated the needles. Others refused antihypertensives because they felt ‘less alive’ on them.
Safety isn’t just about avoiding overdose. It’s about preserving dignity. The real question isn’t ‘how many pills?’ but ‘who are you when you take them?’
I’ve seen too many people feel guilty for forgetting a pill or being scared to ask questions. You’re not dumb. The system is broken.
My mom took 6 meds for years. She never told her cardiologist she was also taking St. John’s Wort because she thought it was ‘just herbal.’ Turns out it tanked her blood thinner’s effect.
Now I go with her to every appointment. I take notes. I ask the hard questions. She says I’m ‘annoying.’ I say I’m her lifeline.
You don’t need to be a doctor to advocate. You just need to show up.
They don’t want you to know this, but Big Pharma *wants* you on 10 meds. Why? Because one pill = one bill. Five pills = five bills. Ten pills = ten bills.
And the ‘medication review’? A joke. They don’t want you to stop anything. They want you to keep refilling.
Ever notice how every drug commercial ends with ‘ask your doctor’? But your doctor gets kickbacks from the reps.
I stopped all my meds. Went keto. Started walking. My BP dropped. My sugar normalized. My doctor panicked. Now he’s trying to get me back on statins.
Wake up. Your body doesn’t need 10 chemicals. It needs rest. Food. Movement. And freedom from corporate control.
Let’s be brutally honest: this article is a Band-Aid on a hemorrhage.
You think the 7 Rights matter when your doctor writes prescriptions in 30 seconds? When your pharmacy fills them with a 14-year-old intern? When your ‘medication review’ is a 5-minute checklist done by a nurse who’s never seen your chart before?
The real problem isn’t patient error. It’s systemic collapse.
Doctors are trained to prescribe, not to coordinate. Pharmacies are incentivized to dispense, not to question. Insurance companies don’t pay for reviews-they pay for refills.
This isn’t about ‘being aware.’ It’s about surviving a broken system that treats you like a data point.
And yet… you’re still expected to memorize 10 pill names, their side effects, and their interactions while juggling jobs, kids, and depression.
That’s not healthcare. That’s a cruel simulation.
I’ve been on the same 4 meds for 12 years. Never missed a dose. Never had a problem. Why? Because I read the pamphlets. I called the pharmacy. I didn’t trust the doctor’s handwriting.
People act like this is some new revelation. It’s not. It’s basic responsibility.
If you can’t manage your meds, don’t blame the system. Blame yourself for being lazy.
My grandfather took 11 pills a day until he was 92. He wrote them down on index cards. He kept them in his wallet. He died peacefully. No hospital. No drama.
It’s not rocket science. It’s discipline.
Hey, I just wanna say-you’re not alone. I was scared to ask my doc about my meds too. Felt like I was bothering him.
Then I wrote down everything on my phone notes. Took a pic. Sent it to him. He replied: ‘Good job. Let’s cut one.’
Turns out I didn’t need the antacid. My stomach was fine. I saved $80/month.
Also, I got a free pill box from my pharmacy. It beeps. I love it. It’s like a little robot friend.
You got this. One pill at a time.
USA. Land of the free. Home of the pill-popping. You think this is bad? Try getting your meds in a red state. One lady in Texas got denied her insulin because her ‘income was too high’ for assistance. She died.
Meanwhile, my cousin got his $2000/month cancer med covered because his dad worked for the drug company. That’s not healthcare. That’s a lottery.
And you wanna talk about ‘7 Rights’? Try ‘Right to Live’ when your meds cost more than your rent.
This isn’t about being smart. It’s about being lucky. And most of us? We’re not.
As a retired nurse who worked in ICU for 35 years, I can tell you: 90% of medication errors happen because the patient didn’t know what they were taking.
Not because they were careless. Because no one explained it.
One man came in with a bag of 17 pills. He didn’t know which was for his heart, which was for his anxiety, which was for his back. He thought they were all ‘vitamins.’
He survived. But only because his daughter found the pharmacy receipt and brought it in.
So please-don’t wait for a crisis. Write it down. Talk to someone. Don’t be shy. Your life isn’t a secret.
Reading these comments, I’m reminded: we’re not just managing drugs. We’re managing fear.
Fear of side effects. Fear of forgetting. Fear of being a burden. Fear of the system failing us.
But here’s what no one says: you are not broken because you need pills.
You are resilient because you keep showing up.
Every time you open that pillbox. Every time you write it down. Every time you speak up-even when your voice shakes.
That’s courage. Not perfection.
Keep going.