When you walk into a doctor’s office, ER, or hospital, the first thing they ask is: "Do you have any drug allergies?" It seems simple. But what you say-and how it’s written down-could literally save your life.
Too many people say, "I’m allergic to penicillin" or "Sulfa makes me sick." But that’s not enough. Vague answers like these lead to dangerous mistakes. A 2019 study in the Journal of the American Medical Informatics Association found that incomplete or wrong allergy records cause about 6.5% of all medication errors. That’s not a small number. It’s enough to put hundreds of thousands of people at risk every year in the U.S. alone.
Why Specificity Matters More Than You Think
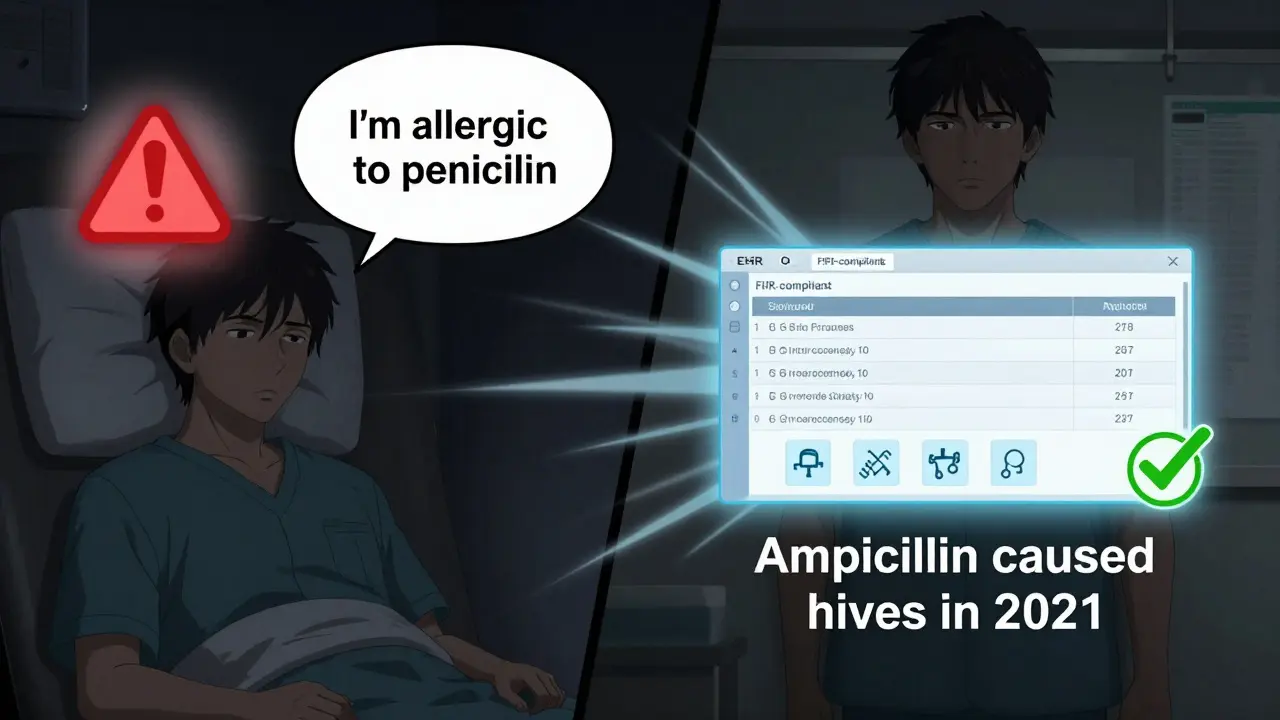
"I’m allergic to penicillin" sounds clear-but it’s not. Penicillin isn’t one drug. It’s a family. Amoxicillin, ampicillin, and others are all part of it. If you only say "penicillin," a doctor might avoid all of them-even if you’ve never reacted to amoxicillin. That means you might get a less effective, more expensive, or more dangerous antibiotic instead.
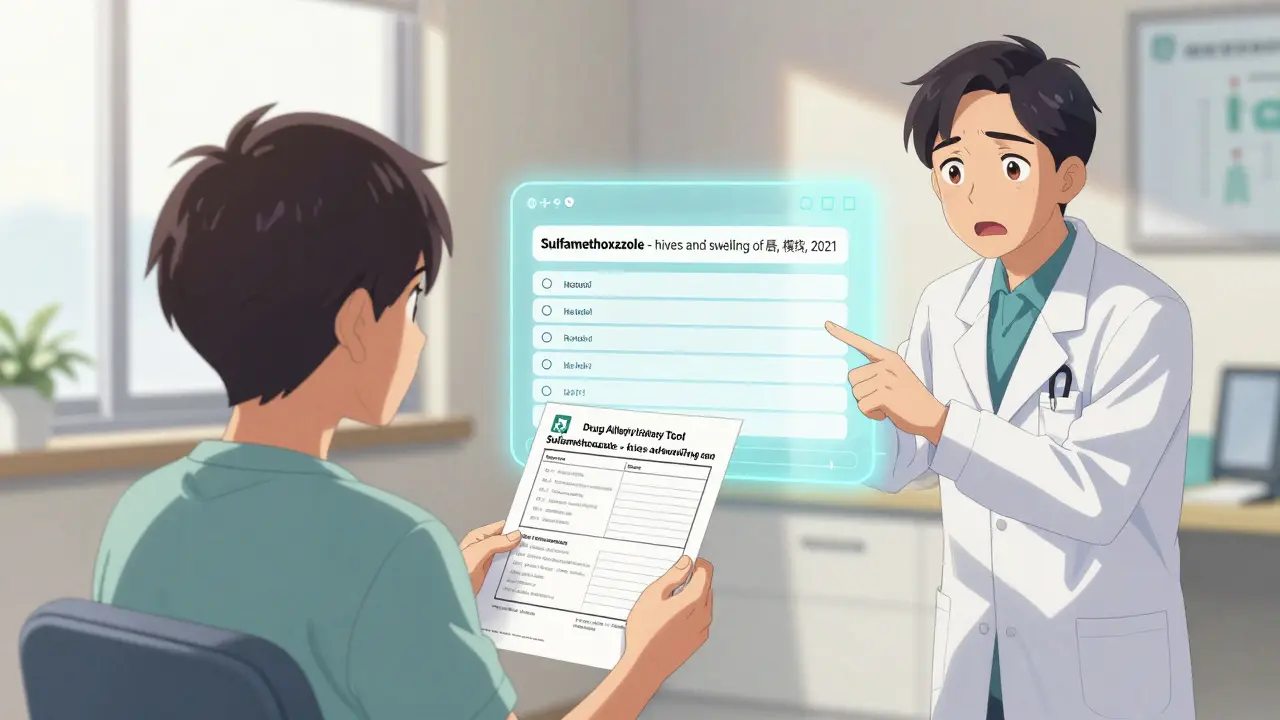
According to the American Academy of Allergy, Asthma & Immunology (AAAAI), you need to document the exact generic name of the drug. Say "ampicillin," not "penicillin." Say "sulfamethoxazole," not "sulfa." Say "ibuprofen," not "Advil." Brand names don’t help. Only the generic name tells the system what you actually reacted to.
And it’s not just the drug. You need to describe what happened. Did you get a rash? Swelling? Trouble breathing? Vomiting? How bad was it? Did it happen right away, or hours later? Did you need epinephrine? Was it life-threatening? All of this matters.
One study at Massachusetts General Hospital found that after a 10-minute structured interview, 61% of patients had their allergy records changed-because what was written down was wrong, vague, or outdated. Over 200 changes were made. That’s not rare. That’s normal.
What Your Medical Record Must Include
By law, your medical record must have a complete, accurate allergy list. It’s not optional. The Centers for Medicare & Medicaid Services (CMS) requires it. The Joint Commission requires it. Your hospital or clinic must follow these rules-or risk losing funding.
Your allergy entry needs four things:
- The drug name (generic only)
- The reaction (rash, hives, anaphylaxis, etc.)
- The severity (mild, moderate, life-threatening)
- The date (when it happened, or if you’re unsure)
Example: "Sulfamethoxazole - hives and swelling of lips, moderate, 2021"
Don’t write "allergic to antibiotics" or "bad reaction to medicine." That’s useless. If you don’t know the drug name, say so. But don’t guess. Say: "I had a reaction to a pill I was given in 2019, but I don’t remember the name."
What About "No Known Allergies"?
If you say you have no drug allergies, that must be written down too. "NKDA" (No Known Drug Allergies) isn’t enough. Your EHR needs to show it clearly as a structured entry. "No allergies" means nothing if it’s buried in a note. Systems need to see it as a confirmed fact-not an assumption.
Even if you’ve never had a reaction, if you’ve never been asked properly, you might be missing something. Many people think they’re allergic because they got a stomachache after taking a pill. But that’s not an allergy. That’s an intolerance. Only a true immune reaction counts as an allergy. And here’s the shocking part: 90-95% of people who say they’re allergic to penicillin aren’t. When tested, they’re fine. But if their record says "penicillin allergy," they’ll be denied the best antibiotic for their infection.
How to Fix Your Own Records
You’re the most important person in this process. No doctor or nurse will dig into your history unless you push them. Here’s what to do:
- Request a copy of your allergy list from your primary care provider or hospital portal. Don’t wait for them to send it.
- Review it carefully. Does it say "penicillin" or "ampicillin"? Does it say "rash" or "anaphylaxis"? Is the date there?
- Call and correct it. Say: "I need to update my allergy record. Here’s what actually happened."
- Ask for a written confirmation. Get an email or printed note that says your record was updated.
- Bring it to every visit. Even if you think they "have it," say: "I want to confirm my allergy list is up to date."
Use a tool like the Drug Allergy History Tool (DAHT) to prepare. It’s a simple questionnaire you can print or fill out on your phone. It asks you exactly what you need to remember: what drug, what happened, how bad, when.
What Happens If You Don’t Document Correctly?
Wrong documentation leads to three big risks:
- Missed treatments: You’re denied the best drug because your record says you’re allergic to something you’re not.
- Wrong substitutions: You get a stronger, costlier, or more toxic drug because the right one was avoided.
- Delayed care: Doctors hesitate, order tests, or avoid prescribing altogether because they’re unsure.
One study showed that when patients had their penicillin allergy properly evaluated and removed from their record, they were 32.7% more likely to get the right antibiotic on the first try. That’s not a small win. That’s better outcomes, fewer hospital stays, and lower costs.
And it’s not just about antibiotics. Allergy errors affect painkillers, anesthesia, chemotherapy, and even vaccines. Any drug can trigger a reaction. And if it’s not documented right, the system won’t protect you.
How Technology Helps (and Hurts)
Most clinics use EHRs like Epic, Cerner, or Meditech. These systems can help-if they’re used right. They can flag potential reactions, warn doctors, and share your info across hospitals.
But here’s the catch: if your allergy is entered as free text-like "had a rash once"-the system can’t read it. It only works if the data is structured: dropdown menus for drug names, checkboxes for symptoms, fields for severity.
Since 2023, federal rules require all certified EHRs to use FHIR standards for allergy data. That means your allergy list should follow the same format whether you’re at a clinic in Minneapolis or a hospital in Miami. But if your doctor just types it in, it doesn’t count.
Computerized alerts reduce errors by up to 55%. But only if the data is accurate. Garbage in, garbage out.
Your Responsibility, Your Safety
Doctors and nurses are busy. They’re not mind readers. They rely on what’s written. If your allergy record is vague, outdated, or missing, you’re the only one who can fix it.
Take five minutes now. Look at your patient portal. Find your allergy list. Is it specific? Is it correct? If not, call your provider. Ask for a review. Ask for help filling out the Drug Allergy History Tool.
Don’t wait for a bad reaction to happen. Don’t assume they "already know." The system doesn’t work unless you make it work.
Your health isn’t a guess. It’s a record. And that record needs to be right.




So let me get this straight - we’re supposed to trust a computer system that can’t even spell ‘accommodate’ right, but now it’s gonna save our lives because we typed ‘sulfamethoxazole’ instead of ‘sulfa’? 😂
Meanwhile, my EHR still thinks I’m allergic to ‘air’ because I sneezed once in 2012. 🤡
If you don’t know your own allergies, you don’t deserve to live.
Let’s be real - this whole ‘structured allergy entry’ thing is just Big Pharma’s way of locking you into their patented antibiotics. 🧪
They don’t want you to know that 95% of ‘penicillin allergies’ are just anxiety + a stomachache.
And guess what? The EHRs? All owned by Epic, which is secretly funded by the same people who own the FDA. 🕵️♂️
They want you scared. They want you dependent.
And now they want you to type in exact generic names like a obedient robot. 🤖
Wake up.
It’s not about safety. It’s about control.
And if you think your ‘allergy record’ is safe? Think again. They’re selling your data to insurers every second. 💸
Don’t be fooled by the ‘FHIR standards.’ That’s just glitter on a prison cell. 🚨
bro why are we even doing this? like i literally just say ‘i’m allergic to stuff’ and they give me tylenol. why do i need to remember some latin word from 2017? 🤡
also who has time to ‘call and correct it’? i got a 9-5 and a kid and a cat that pees on my shoes. this is too much. 😭
The article’s recommendations are clinically sound and align with current standards of care as outlined by the Joint Commission and CMS. Failure to document allergies with specificity constitutes a breach of the standard of care and exposes both patient and provider to unnecessary risk. The data cited is robust and peer-reviewed. No further commentary is required.
Hey, I just checked my portal - my record says ‘penicillin allergy’ but I’ve never had a rash. I’m calling my doctor right now to fix it. But wait - why didn’t my last 3 doctors ask me this? Are they just guessing? I’m gonna email all of them. This is insane. 😡
Also - can someone tell me if ‘allergic to codeine’ counts if I threw up once? I need to know before my next surgery. HELP.
Good post. Really important stuff.
Most people don’t realize how dangerous vague allergy info is - I had a cousin who got clindamycin because they thought she was ‘allergic to penicillin’ and ended up with C. diff. She was in the hospital for 6 weeks.
Just take 5 minutes. Go to your portal. Look at your allergies. If it says ‘penicillin’ - call your doctor. Ask them to check if you’ve ever had a true reaction.
And if you’re not sure? Say so. ‘I don’t remember’ is better than ‘I’m allergic to everything.’
You’re not being difficult. You’re being smart. And your future self will thank you.
Also - the DAHT tool? It’s free. Use it. Print it. Bring it to your next visit. It’s literally one page.
Y’all realize the government’s making us type this stuff so they can track who’s taking what meds, right? 😏
Next thing you know, they’ll flag you as ‘high-risk’ if you ever had a rash after a pill - and then your insurance hikes your rates or denies your surgery.
And Epic? That’s just a front for the NSA. They’ve got your allergy list, your bowel movements, and your TikTok history.
Don’t feed the machine. Just say ‘NKDA’ and move on. 🇺🇸
I once said I was allergic to ‘antibiotics’… and they gave me a steroid shot. I didn’t even know that was an option.
Then I got a rash. Then I got a bill. Then I got confused.
Now I just carry a laminated card that says: ‘I don’t know what I’m allergic to, but I know I hate feeling sick. Please don’t give me anything I didn’t ask for.’
It’s not perfect. But it’s honest.
And hey - if your doctor rolls their eyes? That’s your cue to find a new one.
Also - why does ‘penicillin’ always get all the attention? What about ‘I reacted to that weird purple pill in 2008’? Nobody cares about that. But it could kill you.
…I’m gonna go look at my portal now. Thanks for the nudge.
While the article’s intent is laudable, the underlying assumption that patient-reported data is inherently reliable is empirically flawed. Human memory is fallible, recall bias is pervasive, and the sociological phenomenon of iatrogenic symptom attribution is well-documented in the literature. Furthermore, the imposition of structured data entry protocols without concurrent provider training may exacerbate cognitive load, leading to documentation fatigue and increased error rates. The solution requires systemic reform, not individual compliance.
I just updated my record! 🎉
Used the DAHT tool, found out I never had a real penicillin allergy - just a stomachache after a bad chicken taco in college. 😅
Called my doctor, she was so nice and helped me change it. Now I’m actually eligible for the best antibiotics if I ever get sick.
Thank you for this post - it saved me from a future nightmare.
Also - if you’re reading this and haven’t checked your record yet… please do. It takes 7 minutes. You’ll feel so much better. ❤️
Edith, that’s awesome to hear! 🙌
I’m so glad your doctor helped you - not everyone has that experience. A lot of folks get brushed off. You’re a great example of why patient advocacy matters.
And yeah - chicken taco? Classic false positive. I had one too. After a taco, I thought I was allergic to ‘everything.’ Turns out, it was just the guac.
Keep that updated record safe. And if you ever need help checking another one - I’ve got a template you can use. Just say the word.