
Drug Interaction Checker
Your Current Medications
Separate medications with commas or new lines
New Medication
Results
Enter your medications to check for interactions
This tool helps identify potential interactions but is not a substitute for professional medical advice
Every year in the U.S., thousands of people end up in the hospital-not because their condition got worse, but because a new medication they started reacted badly with something else they were already taking. It could be another pill, a supplement, even grapefruit juice. These are called drug interactions, and they’re one of the most preventable causes of serious harm in modern medicine. The good news? You don’t need to be a doctor to protect yourself. With a few simple, practical steps, you can dramatically reduce your risk.
Why Drug Interactions Matter More Than You Think
A drug interaction happens when one substance changes how another works in your body. This isn’t just about two pills clashing. It’s about how your liver processes drugs, how your kidneys filter them, or how food blocks absorption. Some interactions make a drug useless. Others turn it into a poison. The FDA estimates that preventable adverse drug reactions cause about 7,000 deaths each year in the U.S. And it’s not just seniors. People on multiple prescriptions, those taking supplements, or even folks who grab over-the-counter painkillers without telling their doctor are at risk. A 2022 study found that nearly half of all adverse drug reactions could be avoided with better interaction checking. Take simvastatin (Zocor), a common cholesterol drug. If you also take amiodarone (Cordarone) for heart rhythm, your risk of muscle breakdown-called rhabdomyolysis-jumps 15 times. That can lead to kidney failure or death. This isn’t rare. It’s documented. And it’s preventable.Step 1: Build a Complete Medication List
You can’t check for interactions if you don’t know what you’re taking. Most people think they remember their meds. They don’t. A 2022 survey by the National Community Pharmacists Association found that 68% of patients don’t tell all their doctors about every pill, supplement, or herb they use. Start with a real list-not just your memory. Include:- Every prescription drug, including doses and how often you take them
- All over-the-counter meds: ibuprofen, antacids, sleep aids, cold pills
- Herbal supplements: St. John’s wort, garlic, ginkgo, echinacea
- Vitamins: especially high-dose ones like vitamin K, calcium, or iron
- Any injectables, patches, or inhalers
Step 2: Ask the Right Questions Before Taking Anything New
Don’t just nod and say “yes” when your doctor says, “Here’s a new pill.” Ask these four questions out loud:- Can I take this with my other medications?
- Should I avoid certain foods, drinks, or alcohol?
- What signs of a bad reaction should I watch for?
- How does this drug actually work in my body?
Step 3: Use a Trusted Drug Interaction Checker (But Don’t Rely on It Alone)
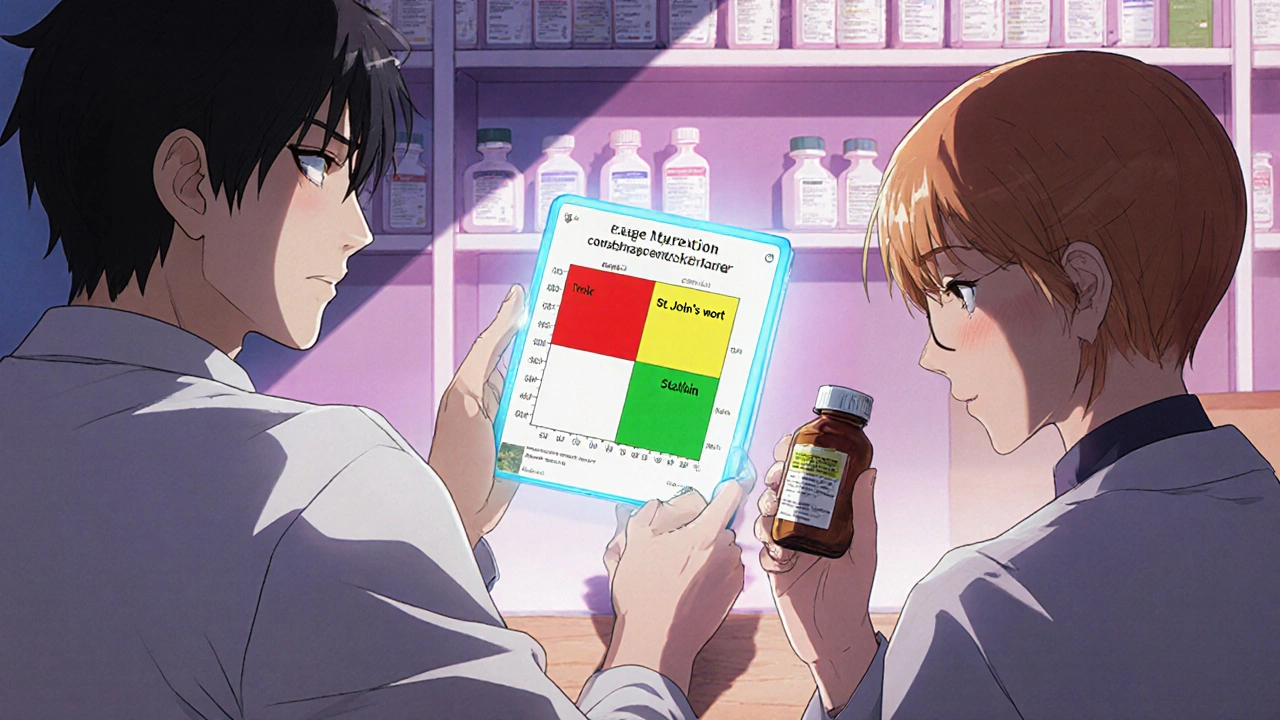
There are free tools online that can help you spot risks. The best ones are updated daily and backed by medical data.- Drugs.com Drug Interactions Checker: Screens over 24,000 prescription drugs, 7,000 supplements, and 4,000 foods. It’s used by over a million people monthly and caught a fatal interaction between sertraline and linezolid that a doctor missed.
- University of Liverpool’s HIV Drug Interaction Checker: Even if you don’t have HIV, this tool is one of the most accurate. It uses a color-coded system: red for dangerous, yellow for caution, green for safe. It rates evidence from 1 (strongest) to 5 (theoretical).
- WebMD’s Tool: Easy to use, but less accurate. Studies show it misses more real interactions than Drugs.com.
Step 4: Know the High-Risk Combinations
Some drug pairs are dangerous more often than others. According to the American Academy of Family Physicians, these seven combinations cause 63% of serious interaction hospitalizations:- Warfarin + NSAIDs (like ibuprofen or naproxen)
- SSRIs (like fluoxetine) + MAO inhibitors (like selegiline)
- Digoxin + clarithromycin (an antibiotic)
- Statins (like simvastatin) + fibrates (like fenofibrate)
- Calcium channel blockers + protease inhibitors (used in HIV treatment)
- Sildenafil (Viagra) + nitrates (like nitroglycerin)
- Theophylline + fluvoxamine (an antidepressant)
Step 5: Use One Pharmacy for Everything
This is one of the simplest, most powerful things you can do. When you use multiple pharmacies, each one only sees part of your medication picture. That’s how dangerous combinations slip through. A 2021 study of 22,000 Medicare patients found that using just one pharmacy cuts serious drug interactions by 31%. Why? Because that one pharmacy can run a full check across all your prescriptions, OTC meds, and supplements. The catch? Only 38% of Americans stick with one pharmacy. Most switch for lower prices or convenience. But saving $10 on a prescription isn’t worth a trip to the ER.Step 6: Watch for Red Flags
Even with all the checks, things can still go wrong. Know what to look for:- Sudden dizziness, fainting, or confusion
- Unexplained bruising or bleeding
- Severe muscle pain or weakness (especially with statins)
- Heart palpitations or irregular heartbeat
- Swelling in your hands, feet, or face
- Severe nausea, vomiting, or diarrhea
Step 7: Keep a Medication Passport
The Cleveland Clinic calls it a “medication passport”-a simple document you update after every doctor visit, pharmacy refill, or ER trip. Keep it in your wallet or phone. Include:- Your full medication list
- Allergies
- Chronic conditions (diabetes, kidney disease, etc.)
- Emergency contact
What About Supplements and Natural Remedies?
People think “natural” means safe. It doesn’t. St. John’s wort can make birth control, antidepressants, and even some cancer drugs useless. Garlic and ginkgo can thin your blood-dangerous if you’re on warfarin or about to have surgery. Turmeric can interfere with blood sugar meds. Green tea extract can affect liver enzymes. A 2023 survey found that 58% of patients never tell their doctor about supplements. That’s a huge blind spot. Always disclose everything-even if you think it’s “just a tea.”Technology Is Helping, But You’re Still the Last Line of Defense
Hospitals and pharmacies now use computer systems that flag interactions. But even with 92% of U.S. pharmacies using these tools, pharmacists still filled dangerous prescriptions in 8.3% of cases-mostly when patients used multiple pharmacies. New AI tools are getting better. The FDA’s pilot program uses machine learning to predict your personal risk based on your health record. Early results show 89% accuracy-far better than old rule-based systems. But none of this matters if you don’t speak up. If your doctor doesn’t ask about your supplements, tell them. If your pharmacist doesn’t flag something, ask why. You’re the only person who knows your whole story.Frequently Asked Questions
Can grapefruit really interfere with my medications?
Yes. Grapefruit and grapefruit juice can block enzymes in your liver that break down certain drugs. This causes the drug to build up to dangerous levels. It’s especially risky with statins (like simvastatin), blood pressure meds (like amlodipine), and some anti-anxiety drugs. Even one glass can cause problems that last 24 hours. If you’re on a medication that interacts with grapefruit, avoid it completely.
What if my doctor says a combination is safe, but the online checker says it’s not?
Always bring it up again. Doctors aren’t always aware of the latest interaction data, especially with supplements or newer drugs. Ask your doctor to explain why they think it’s safe. Request a second opinion from your pharmacist-they’re drug experts and often catch what others miss. Don’t take a risk just because one person said it’s okay.
Are herbal supplements regulated like prescription drugs?
No. The FDA doesn’t test herbal supplements for safety, purity, or interactions before they’re sold. A supplement labeled as “pure” might contain hidden drugs, contaminants, or inconsistent doses. A 2020 study found that nearly 20% of herbal products contained unlisted pharmaceutical ingredients. Always assume supplements can interact-and tell your doctor about them.
How often should I review my medication list?
At least once a year, or anytime you start or stop a medication-even if it’s just a cold pill. Many people don’t realize that a short-term antibiotic or painkiller can still interact with a daily blood pressure pill. Bring your list to every appointment, even routine checkups. Your body changes over time, and so can how your meds work.
What should I do if I accidentally take two interacting drugs?
Don’t panic, but act fast. Call your pharmacist or doctor right away. If you’re having symptoms like chest pain, trouble breathing, severe dizziness, or muscle weakness, go to the ER. Don’t wait. Some interactions take hours to show effects, but others can turn dangerous within minutes. Keep your medication list handy when you call-it helps them give you better advice.
Next Steps: Make a Plan Today
Here’s what to do before your next doctor visit:- Write down every medication, supplement, and vitamin you take.
- Bring the actual bottles to your appointment.
- Use Drugs.com to check for interactions between your current meds and anything new your doctor suggests.
- Ask your pharmacist if you can switch to one pharmacy for all your prescriptions.
- Make a printed medication passport and keep it in your wallet.



I used to think supplements were harmless until my grandma ended up in the ER after mixing St. John’s wort with her blood pressure med. Now I bring every bottle to every appointment-no exceptions. This guide? Spot on. Simple, practical, and life-saving.
OMG, YES!! I literally just started a new antidepressant last week and didn’t even think to ask about grapefruit juice-I drink it every morning!! I’m going to call my pharmacist RIGHT NOW!! Also, I’ve been taking turmeric for ‘inflammation’-is that bad?? I’m so scared now!!
As someone who grew up in a household where ‘natural remedies’ were gospel, I didn’t realize how dangerous some of these ‘harmless’ herbs could be. My mom took ginkgo with her warfarin for years-no one told her it was risky. This post opened my eyes. We need more of this kind of education, especially in communities that distrust Western medicine. Knowledge isn’t just power-it’s survival.
Effective medication management requires diligence, consistency, and communication. The seven-step framework outlined here aligns with evidence-based clinical guidelines. Utilizing a single pharmacy and maintaining a physical medication list are two of the most statistically significant interventions for reducing adverse drug events. I recommend all patients adopt these practices without delay.
bro i just realized i’ve been taking melatonin with my blood pressure med for 2 years… i’m gonna throw my whole cabinet out and start over. also why is no one talking about how weird it is that we have to be detectives just to not die from pills?? this system is broken
One might posit that the true pathology lies not in the pharmacological interactions themselves, but in the epistemological disconnect between patient agency and institutional medical authority. The proliferation of drug interaction checkers, while technologically laudable, reflects a systemic abdication of responsibility by clinicians to educate. The patient, thus, becomes the reluctant pharmacist of their own physiology-a condition both tragic and absurd.
Just want to add: if you're on any statin (like simvastatin or atorvastatin), avoid grapefruit COMPLETELY-even a little bit. I had a patient who drank half a glass on Sunday and was hospitalized Tuesday with rhabdo. Also, if you're on warfarin, don't suddenly start eating kale smoothies every day-vitamin K flips your INR like a switch. And yes, your pharmacist WILL know this stuff better than your doctor-ask them. They’re the unsung heroes of safe med use.
Man, this hits different in India too. People here take ashwagandha like candy, mix it with diabetes meds, and wonder why their sugar crashes. My uncle ended up in ICU because he took turmeric with his blood thinner-thought it was ‘just a spice.’ We need more of this awareness in non-Western countries too. Maybe someone should translate this into Hindi, Bengali, Tamil… this info should be everywhere.
U.S. healthcare is a joke. You need a PhD just to not die from a pill. Why does the government let this happen? In Canada, pharmacists review ALL meds before dispensing-no exceptions. Here? You’re on your own. And they wonder why people hate doctors.
You’re all being too nice. This is a scam. Doctors don’t care. Pharmacies don’t care. You think they want you to know this? No. They make money when you get sick. Just stop taking everything. Just eat vegetables. That’s the real answer.