
When your lungs can’t get enough oxygen, your heart has to work harder. But when that strain becomes constant, it doesn’t just tire out your heart-it starts to break it. Pulmonary hypertension (PH) isn’t just high blood pressure in the lungs. It’s a silent, progressive disease that slowly overloads the right side of your heart, leading to failure if left unchecked. Many people mistake its early signs for asthma, aging, or being out of shape. By the time they get a real diagnosis, the damage is often advanced. But understanding the symptoms, recognizing right heart strain, and knowing what treatments actually work today can change everything.
What Pulmonary Hypertension Really Means
Pulmonary hypertension means the blood pressure in the arteries leading from your heart to your lungs is too high. Normal pulmonary artery pressure is around 8-20 mmHg at rest. When it climbs above 20 mmHg, that’s the official cutoff for PH, as updated by the World Health Organization in 2018. This isn’t just a number-it’s a warning sign your heart is struggling to push blood through stiff, narrowed, or blocked lung vessels.
PH isn’t one disease. It’s grouped into five types based on cause. Group 1, pulmonary arterial hypertension (PAH), affects the small arteries in the lungs directly. Group 2 comes from left heart failure. Group 3 is tied to lung diseases like COPD or pulmonary fibrosis. Group 4 is caused by blood clots in the lungs that never dissolve. Group 5 includes rare cases with unclear causes, like blood disorders or metabolic diseases. Knowing the group matters because treatment changes drastically depending on what’s driving it.
Early Symptoms Are Easy to Miss
The first symptom? Shortness of breath. But not the kind you get after climbing stairs. This is breathlessness that creeps up during simple tasks-walking to the mailbox, tying your shoes, even sitting still. It’s out of proportion to your fitness level. You might feel fine when you’re resting, but your body tells you something’s wrong when you move.
Other early signs include fatigue that doesn’t go away, a racing heartbeat, and swelling in your ankles or legs. Some people feel lightheaded or pass out during activity. These aren’t normal. Yet, in a 2023 survey by the Pulmonary Hypertension Association, 78% of patients reported being told they had asthma or COPD before getting the right diagnosis. The average delay? Nearly three years.
Doctors often miss PH because it’s rare and symptoms overlap with common conditions. But there are red flags: unexplained right ventricular hypertrophy on an EKG, persistent swelling without heart failure, or worsening breathlessness despite normal lung function tests. If you’ve had these for months and nothing’s helping, push for further testing.
Right Heart Strain: The Hidden Killer
Every time your right ventricle pumps blood into the lungs, it fights against high pressure. Over time, the muscle thickens, stretches, and weakens. This is right heart strain-and it’s what turns PH from a lung problem into a life-threatening heart condition.
Doctors look for three key signs on echocardiograms:
- Right ventricular wall thickness over 5 mm
- Right ventricular dilation-an end-diastolic area larger than 22 cm²
- TAPSE less than 17 mm, which means the heart’s pumping ability is dropping
These aren’t just numbers. They predict survival. A TAPSE under 17 mm doubles your risk of death within a year. A 6-minute walk test distance under 380 meters is another major red flag-it means your body can’t handle basic activity without oxygen starvation.
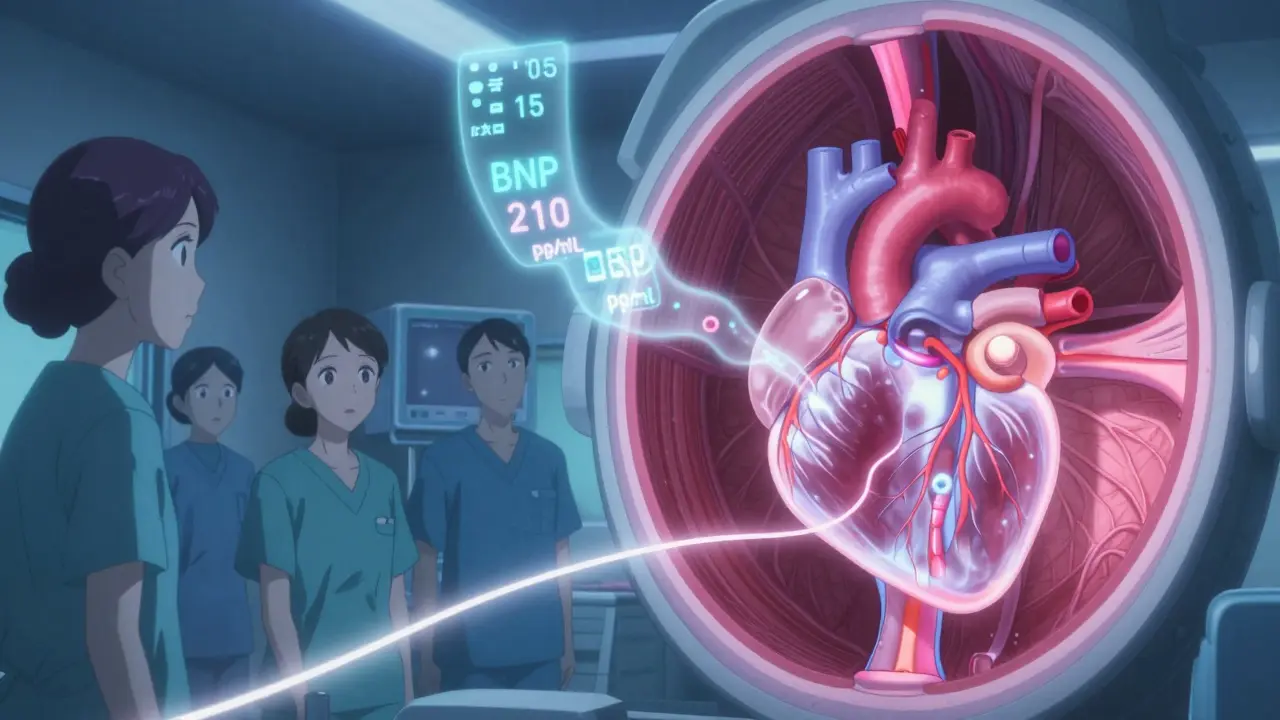
Biomarkers like BNP and NT-proBNP also tell the story. If your BNP is above 180 pg/mL or NT-proBNP above 1,400 pg/mL, your right heart is under serious stress. These levels correlate strongly with how close you are to heart failure.
And here’s the scary part: the right ventricle doesn’t show symptoms until it’s failing. By the time you feel chest pain or severe swelling, the damage is often advanced. That’s why monitoring these signs-even if you feel okay-is critical.
Diagnosis Isn’t Simple-But It’s Necessary
Echocardiograms are the first step. They’re non-invasive, widely available, and can estimate pulmonary pressure. But they’re not perfect. Studies show they overestimate pressure by 10-15 mmHg in over half the cases. A reading of 40 mmHg might mean your real pressure is only 25. Or worse-it might be 50.
The only way to know for sure is right heart catheterization. This is the gold standard. A thin tube is threaded from your neck or groin into your heart to directly measure pressure in the pulmonary arteries. It’s the only test that can tell you if your PH is pre-capillary (Group 1 or 4) or post-capillary (Group 2). That distinction changes everything in treatment.
Yes, it’s invasive. There’s a small risk of complications: arrhythmia (3.4%), pneumothorax (1.2%), or bleeding (5.7%). But the risk of misdiagnosis is far higher. Dr. Nazzareno Galiè, a leading expert, says: “Non-invasive methods cannot replace direct pressure measurement.”
For patients with complex cases, cardiac MRI gives the clearest picture of right ventricular size and function. But it’s only available at about one-third of PH centers. So for most, echocardiography and catheterization remain the backbone of diagnosis.
Therapy Has Changed Dramatically
Twenty years ago, PH was a death sentence. Median survival after diagnosis was just 2.8 years. Today, with modern therapy, 5-year survival is over 60%. That’s not luck-it’s science.
There are now 14 FDA-approved drugs for PH, grouped into five classes:
- Endothelin receptor antagonists (bosentan, macitentan)
- Phosphodiesterase-5 inhibitors (sildenafil, tadalafil)
- Prostacyclin pathway agents (epoprostenol, treprostinil, selexipag)
- Soluble guanylate cyclase stimulators (riociguat)
- Novel TGF-β inhibitors (sotatercept, approved in 2021)
Most patients today start on combination therapy-not just one drug. The REVEAL Registry found 68% of PAH patients are on two or more medications at diagnosis. This multi-target approach works better because PH affects multiple pathways in the body.
Sotatercept is a game-changer. It’s the first drug that doesn’t just widen blood vessels-it actually reverses the abnormal growth in lung arteries. In the STELLAR trial, it cut the risk of death or clinical worsening by 44%. It’s not a cure, but it’s the closest thing we’ve had in decades.
For Group 4 PH (chronic thromboembolic disease), surgery called pulmonary thromboendarterectomy (PTE) can be curative. But it’s only done at specialized centers. If you have PH from old clots, ask if you’re a candidate.
Why Specialized Centers Matter
There are only about 35 certified PH centers in the entire United States. They treat 75% of patients. Why? Because managing PH isn’t just about giving pills. It’s about coordinated care.
A top PH clinic includes a pulmonologist, cardiologist, pharmacist, nurse coordinator, and social worker. Nurse coordinators reduce hospitalizations by 27%, according to the COMPERA registry. They track your walk distance, BNP levels, and echo results. They help you navigate insurance-because getting approved for IV prostacyclin can take over 30 days, and many patients delay treatment because of it.
Doctors at these centers also know how to interpret hemodynamic data correctly: pulmonary vascular resistance over 3 Wood units, transpulmonary gradient above 12 mmHg, diastolic pressure gradient over 7 mmHg. These numbers tell them what type of PH you have-and what drugs will work.
If you’re diagnosed with PH, ask: “Is my care team certified by the Pulmonary Hypertension Care Center program?” If not, get a referral. Your survival depends on it.
What’s Next? The Future of PH Care
The 2022 update to diagnostic criteria lowered the pressure threshold from 25 to 20 mmHg. That means more people will be diagnosed earlier. But that also means more people need access to care-and that’s where the system fails.
A 2023 AHRQ report found minority patients wait 47% longer for diagnosis and have 32% higher mortality rates. Insurance denials, lack of specialist access, and provider unawareness all play a role. The Pulmonary Hypertension Association’s 2025 plan aims to cut diagnostic delays to under a year by training primary care doctors to spot the red flags.
On the research side, new biomarkers like let-7 microRNA are being tested to catch right heart strain before symptoms appear. Drugs targeting right ventricular metabolism, like dichloroacetate, are in phase 2 trials. These could help the heart use energy more efficiently instead of burning out.
But the biggest breakthrough won’t come from a drug. It’ll come from catching PH sooner-before the heart breaks.
What You Can Do Now
If you have unexplained shortness of breath, swelling, or fatigue that doesn’t improve:
- Ask your doctor for an echocardiogram
- Request a 6-minute walk test
- Get your BNP or NT-proBNP checked
- If any of these are abnormal, insist on referral to a PH specialist
Don’t wait for symptoms to get worse. Don’t accept “it’s just aging” or “you’re out of shape.” PH doesn’t care how fit you are. It only cares if you get diagnosed early enough to stop it.



ph is just asthma but the docs are too lazy to do a cath. also bnp is garbage if you’re dehydrated. 🤷♀️
Ah yes, the sacred ritual of right heart catheterization-wherein we stick a tube into a living human being because *maybe* the echo was off by 15 mmHg. How quaint. We’ve got AI-powered echocardiography now, yet we still treat patients like 19th-century lab rats. The medical-industrial complex thrives on unnecessary procedures. 🌹
The assertion that echocardiography overestimates pressure by 10–15 mmHg in over half of cases is statistically unsound. A 2021 meta-analysis in the Journal of the American College of Cardiology demonstrated a mean absolute error of 4.3 mmHg, with 95% CI ±6.1. The author’s rhetoric is alarmist and lacks evidentiary rigor.
They’re hiding the truth. The FDA approved sotatercept because Big Pharma owns the WHO now. Also, why do all these specialists live in NYC? 🤔🇺🇸 #PHConspiracy
I had a cousin in Texas who was told she had 'just bronchitis' for 4 years. Finally got diagnosed at a PH center in Houston-now she’s hiking the Appalachian Trail. It’s not magic. It’s access. If you’re not near a center, you’re playing Russian roulette with your heart.
I’m so sick of people saying ‘it’s just aging’-NO. IT’S NOT. IT’S NOT. IT’S NOT. If you’re tired walking to the fridge at 50, that’s not a midlife crisis-that’s your right ventricle screaming for help. Get tested. NOW.
The entire PH diagnostic framework is built on flawed hemodynamic assumptions. TAPSE is a relic. BNP is influenced by renal function, BMI, and even time of day. They’re treating numbers, not people. This isn’t medicine-it’s data worship.
I think what’s beautiful here is how the body whispers before it screams. We’ve trained ourselves to ignore the quiet signals-fatigue, slight swelling, that odd breathlessness after tying shoes. Maybe the real breakthrough isn’t a drug… but learning to listen again.
Sotatercept? Hell yes. I’ve seen patients go from 6-minute walk of 210m to 480m in 6 months. It’s not just vasodilation-it’s like the lungs are getting a fresh coat of paint. Also, if you’re on IV epoprostenol and your pump beeps? Don’t ignore it. I’ve seen people die because they thought 'it’ll wait till morning.' It won’t.
There’s a deeper philosophical layer here: if we define disease by a number-20 mmHg, 17 mm TAPSE, 1400 pg/mL NT-proBNP-then are we not reducing human suffering to a spreadsheet? The heart doesn’t care about WHO guidelines. It just wants to pump. Maybe the real treatment is restoring dignity to the patient’s lived experience, not just correcting lab values.
Of course they’re pushing sotatercept-it’s $500,000 a year. Meanwhile, my sister was denied insurance for treprostinil because she 'didn’t meet severity thresholds.' They don’t want to cure PH. They want to monetize it. And the doctors? They’re just the middlemen in a gilded cage.
So here’s the thing: if you’ve got unexplained fatigue and your doc says 'go to the gym,' run. Not walk-run. Because that’s not laziness. That’s your right ventricle crying for help. And if they won’t order an echo? Go to urgent care. Demand it. You’re not being dramatic. You’re being smart.