
Clozapine Dose Adjustment Calculator
If you're taking clozapine for treatment-resistant schizophrenia, smoking affects your medication levels. This calculator helps determine the appropriate dose adjustment when starting or quitting smoking based on clinical guidelines.
Why Your Clozapine Dose Might Need to Change If You Smoke
If you're taking clozapine for treatment-resistant schizophrenia, and you smoke tobacco, your body is processing your medication differently than someone who doesn’t smoke. This isn’t just a minor detail-it’s one of the most important drug-environment interactions in psychiatry. Smoking can slash your clozapine blood levels by 30% to 50%, which means your symptoms could come back even if you’re taking the same dose you’ve been on for months.
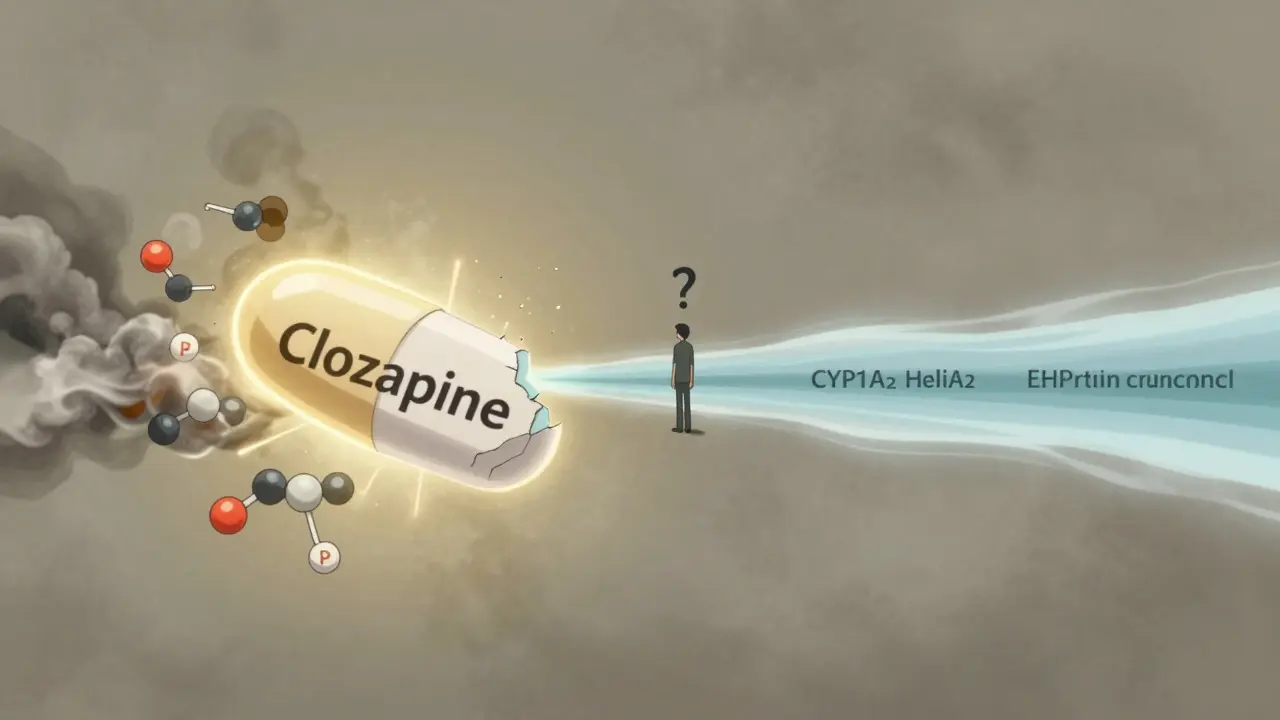
How Tobacco Changes How Your Body Handles Clozapine
Clozapine is broken down mostly by an enzyme in your liver called CYP1A2. When you smoke tobacco, chemicals like polycyclic aromatic hydrocarbons enter your body and trigger your liver to make more of this enzyme. More enzyme means your body clears clozapine faster. The result? Lower levels in your blood. You might not feel any different at first, but over days or weeks, your medication stops working as well.
This isn’t a slow process. If you start smoking regularly, your clozapine levels begin dropping within 48 to 72 hours. And if you quit? The enzyme doesn’t disappear overnight-it takes one to two weeks to return to normal. That’s why people who stop smoking while staying on the same clozapine dose often end up with toxic levels, leading to dizziness, seizures, heart problems, or worse.
It’s Not Just Cigarettes-Vaping Does This Too
Many people assume e-cigarettes or vaping are safer when it comes to medication interactions. But research from the University of Toronto in 2024 shows that vaping also induces CYP1A2. It’s not quite as strong as tobacco smoke-maybe 15% to 20% less-but it’s still enough to lower clozapine levels. If you switched from cigarettes to vaping thinking you’d avoid this problem, you haven’t. Your doctor still needs to know.
Why Clozapine Is Different From Other Antipsychotics
Not all antipsychotics react this way. Olanzapine is also affected by smoking, but less dramatically. Risperidone? Barely affected. Why? Because clozapine relies on CYP1A2 for 60% to 70% of its clearance. For most other drugs, that number is under 40%. Add to that clozapine’s narrow therapeutic range-between 350 and 500 ng/mL-and you’ve got a recipe for trouble.
Too low? Your psychosis returns. Too high? You risk seizures, heart rhythm problems, or agranulocytosis (a dangerous drop in white blood cells). That’s why doctors don’t just guess your dose-they measure it. Therapeutic drug monitoring isn’t optional with clozapine. It’s mandatory.
What Happens When You Start or Stop Smoking
Let’s say you’ve been on 300 mg of clozapine daily for a year. Your levels are steady at 420 ng/mL. You start smoking. Two weeks later, your levels drop to 180 ng/mL. Your hallucinations come back. You think the medication stopped working. You don’t tell your doctor. You increase your dose on your own. Now you’re at 400 mg, but your levels are still low because your body is still clearing the drug fast.
Now flip the scenario. You quit smoking cold turkey. Your doctor doesn’t reduce your dose. After 10 days, your clozapine level spikes to 800 ng/mL. You’re extremely sleepy, your heart races, you can’t stand up without feeling dizzy. You end up in the ER. That’s not a rare event. Case reports show this happens dozens of times every year across the U.S.
Real-world data from Doximity in 2023 shows that 82% of psychiatrists who treat clozapine patients adjust doses when smoking status changes. And 68% check smoking status at every visit. If your doctor isn’t doing this, ask why.
Genetics Play a Role Too
Not everyone who smokes sees the same drop in clozapine levels. Some people are genetically wired to respond more strongly to tobacco’s effect on CYP1A2. The CYP1A2 *1F/*1F genotype, for example, doesn’t change your baseline enzyme activity-but it makes you way more sensitive to induction from smoking. One 2024 case report showed a patient with this genotype needed a 70% dose increase after starting to smoke, while others with the same habit only needed 40%.
Genetic testing for CYP1A2 isn’t routine yet, but it’s becoming more common. In 2018, only 15% of U.S. academic centers tested for it. By 2023, that number jumped to 47%. If you’re struggling to find the right dose, ask your doctor if genotyping could help.
What You Should Do Right Now
- If you smoke: Tell your prescriber. Don’t wait for your next appointment. Call today.
- If you’ve recently quit smoking: Tell your prescriber. Your dose may need to come down.
- If you’re thinking about quitting: Don’t do it without talking to your doctor first. Quitting cold turkey while staying on your current clozapine dose is dangerous.
- Get your blood levels checked: If you haven’t had a clozapine level test in the last 3 months, request one.
- Keep a log: Note when you started or stopped smoking, when your dose changed, and how you’ve been feeling.
What Your Doctor Should Be Doing
Good clinical practice means:
- Checking clozapine levels before any dose change.
- Rechecking levels 4 to 7 days after a dose adjustment.
- Increasing dose by 40% to 60% when a patient starts smoking (e.g., from 300 mg to 450-500 mg).
- Reducing dose by 30% to 50% when a patient quits smoking (e.g., from 500 mg to 250-350 mg).
- Monitoring for signs of toxicity or relapse for at least two weeks after a change in smoking status.
Many electronic health records now have built-in alerts for this interaction. A 2023 study in JAMA Internal Medicine found that hospitals using these alerts reduced clozapine-related adverse events by 37%. If your doctor’s system doesn’t flag this, it’s worth bringing up.
What If You Can’t Quit Smoking?
Smoking is hard-especially with schizophrenia. The rate of tobacco use among clozapine patients is 60% to 70%. That’s nearly five times higher than the general U.S. population. But quitting isn’t the only solution.
If you’re stable on clozapine and smoking, your doctor might choose to keep you on a higher dose rather than push you to quit. That’s not giving up. It’s managing your illness effectively. The goal isn’t to punish you for smoking-it’s to keep you safe and symptom-free.
There are also new formulations in development. A 2024 clinical trial is testing a slow-release clozapine pill designed to smooth out the peaks and valleys caused by CYP1A2 induction. Early results show 40% less variability in blood levels among smokers. That could be a game-changer.
Other Medications That Interfere
Smoking isn’t the only thing that cranks up CYP1A2. Some seizure meds like oxcarbazepine do too. Even certain herbal supplements can. If you’re taking anything else-prescription, over-the-counter, or natural-tell your doctor. Multiple inducers can multiply the effect.
And while clozapine is the most sensitive, olanzapine is also affected. If you’re on olanzapine and smoke, your dose might need a small tweak. But the risk isn’t nearly as high as with clozapine.
The Bigger Picture: Why This Matters
Unmanaged clozapine-smoking interactions lead to 22% higher hospitalization rates, costing about $14,500 per avoidable stay. That’s not just a medical issue-it’s an economic one. The National Institute of Mental Health awarded $2.3 million in 2022 just to study how to fix this.
And yet, most patients aren’t warned. Most doctors don’t check levels often enough. Most insurance plans don’t cover routine clozapine monitoring. This isn’t about blame. It’s about awareness. You deserve to know how your habits affect your treatment.
Final Thought: You’re Not Alone
Thousands of people on clozapine smoke. Thousands more have tried to quit and ended up in crisis because their dose wasn’t adjusted. You’re not failing because you smoke. You’re not weak because you need a higher dose. You’re someone managing a complex illness in a world that doesn’t always understand the science behind it.
What matters is that you’re here, reading this. That means you’re taking control. Talk to your doctor. Get your levels checked. Don’t wait for a crisis to change something.
Does smoking really lower clozapine levels by 50%?
Yes, studies show that smoking can reduce clozapine blood levels by 30% to 50%, with some individuals seeing even greater drops. This happens because tobacco smoke activates the CYP1A2 enzyme, which breaks down clozapine faster. The FDA and major psychiatric guidelines recognize this as a clinically significant interaction.
What should I do if I want to quit smoking while on clozapine?
Don’t quit without talking to your doctor first. When you stop smoking, your CYP1A2 enzyme activity slows down over 1-2 weeks. If your clozapine dose stays the same, your blood levels can rise dangerously-leading to sedation, seizures, or heart issues. Your doctor will likely reduce your dose by 30% to 50% and monitor your levels closely during this time.
Are e-cigarettes safer than cigarettes for clozapine users?
No. Research from 2024 shows that e-cigarettes also induce CYP1A2, though slightly less than traditional cigarettes. If you vape, your clozapine levels may still drop. You still need to tell your doctor and get your levels checked.
How often should clozapine levels be checked?
The American Psychiatric Association recommends checking clozapine levels before starting the medication, then every 3-6 months if stable. But if your smoking status changes, check levels 4-7 days after any dose adjustment. Many experts recommend checking at every visit if you smoke or have recently quit.
Can I switch to another antipsychotic to avoid this problem?
Some antipsychotics like aripiprazole or quetiapine aren’t broken down by CYP1A2, so smoking doesn’t affect them as much. But clozapine is the most effective medication for treatment-resistant schizophrenia. If other drugs haven’t worked, switching might mean losing control of your symptoms. Talk to your doctor about whether switching is right for you.
Is genetic testing for CYP1A2 worth it?
It’s not required, but it can help. People with the CYP1A2 *1F/*1F genotype are more sensitive to tobacco’s effects. If you’ve had trouble finding the right dose despite consistent smoking habits, genetic testing might explain why. It’s becoming more available at major psychiatric centers.



So let me get this straight-smoking cuts clozapine levels by half, but nobody tells you until you're hallucinating again? Classic. My shrink didn't even mention this until I started coughing up lungs and my meds stopped working. Now I'm on 500mg and still feel like a zombie. Thanks, healthcare system.
This is why we need better patient education. If you're on clozapine and smoke, your doctor should be checking levels every time you walk in. No excuses.
I can't believe people still smoke?! Like, are you TRYING to kill yourself?! I quit vaping last year and my meds finally worked-my psychiatrist cried. You're not weak for needing a higher dose-you're just not trying hard enough!!!
The real tragedy isn't the enzyme induction-it's the systemic neglect. We treat psychiatric patients like broken machines that need recalibration, not human beings with biological variability. The fact that this interaction is still under-discussed speaks volumes about how little we value mental health as actual medicine. CYP1A2 isn't just a metabolic pathway-it's a mirror of our societal indifference.
Lmao, people still think vaping is 'safe' for clozapine? Bro, it's still nicotine + flavor chemicals = CYP1A2 induction. I'm Indian, we've been smoking bidi for generations, and my cousin's clozapine dose went from 300 to 650mg after he switched to vape pens. Don't be fooled by marketing.
If you're reading this and you're on clozapine, please call your doctor today. No, not tomorrow. Today. Your life could depend on it. You're not being dramatic-you're being smart.
The use of the phrase 'you're not weak' is dangerously sentimental. It infantilizes patients. The issue is not emotional validation-it is pharmacokinetic precision. If your plasma concentration falls below 350 ng/mL, your psychosis will return. Period. No motivational posters required.
I just quit smoking after 12 years and my doc lowered my clozapine by 40%... I'm not gonna lie, I felt like a ghost for a week 😭 But now I'm lucid for the first time in years. Thank you, science. 🙏
I've been on clozapine for 8 years. I smoke. My levels are monitored every 6 weeks. My doctor uses an alert system built into our EHR. It's not hard. It's not expensive. It's just not done everywhere. If your provider isn't doing this, find someone who will.
Aussie here. We don't have this problem because our health system doesn't let people smoke and get antipsychotics without a lung scan and a sobriety contract. You Americans are just too lazy to enforce basic safety protocols.
I work in a psychiatric clinic. We had a patient last month who went into cardiac arrest after quitting smoking cold turkey. His clozapine level was 920 ng/mL. He survived. He's now on 200mg. This isn't theoretical. It's happening every day. Please, if you're reading this-tell your provider.
The CYP1A2 *1F/*1F genotype is not merely a pharmacogenetic curiosity-it is a clinically actionable biomarker. The absence of routine genotyping in clinical practice constitutes a deviation from the standard of care. The American Psychiatric Association must issue a formal guideline mandating CYP1A2 screening for all clozapine initiates, particularly those with a history of tobacco use.
I'm a nurse in a psych unit. I've seen this happen too many times. One guy started smoking after discharge, doubled his dose himself, ended up in ICU. Another quit smoking, didn't tell anyone, got seizures. Please-don't be the next case study. Talk to your doctor. Seriously.
I've been thinking about this for weeks. The CYP1A2 enzyme isn't just a metabolic switch-it's a biological negotiation between environment and genetics. Smoking doesn't just alter drug levels; it alters the very relationship between the self and the medication. We treat clozapine like a fixed dose, but it's actually a dynamic dialogue with your body, your habits, your trauma, your biology. The real question isn't 'how much do I need?' but 'who am I becoming as I take this pill?' And if smoking is part of my coping, does lowering the dose mean I have to give up that part of myself too? Or is the real solution a slower-release formulation that lets me be both medicated and human?
If you're on clozapine and smoke, your doctor needs to know. If you quit smoking, your doctor needs to know. If you vape, your doctor needs to know. If you take St. John's Wort, your doctor needs to know. If you're on carbamazepine, your doctor needs to know. This isn't optional. This isn't advice. This is survival. Get your levels checked. Every. Single. Time. Your life is worth more than your pride.