
Drug shortages aren’t just inconvenient-they’re dangerous. When a life-saving antibiotic or heart medication runs out, hospitals scramble. Patients delay treatment. Some don’t get help in time. This isn’t a rare event. In 2024, the FDA recorded over 300 drug shortages in the U.S. alone. And the root cause? Fragile pharmaceutical supply chains that rely too heavily on a few overseas factories. The good news? We know how to fix this. Building a resilient pharmaceutical supply chain isn’t about going completely local. It’s about smart planning, smarter tech, and real preparation.
Why Your Medicine Might Not Be There Tomorrow
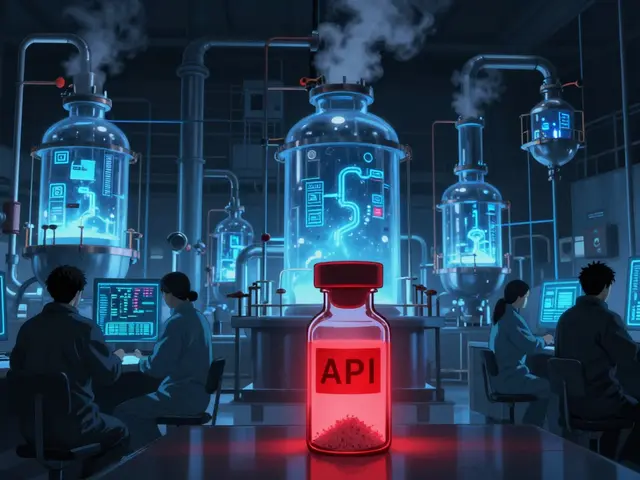
Most people don’t realize that 80% of the active ingredients in U.S. drugs come from just two countries: China and India. That’s not a coincidence-it’s the result of decades of cost-cutting. Factories overseas can produce active pharmaceutical ingredients (APIs) cheaper than U.S. plants. But that efficiency came at a price. When a factory in China shuts down because of a flood, a political dispute, or a quality failure, the ripple effect hits American pharmacies within weeks. The FDA says 40% of finished drug products are also made overseas. One disruption, and entire classes of medications vanish from shelves. Sterile injectables? Only 12% are made in the U.S. Antibiotics? Just 17%. These aren’t niche drugs-they’re the ones hospitals rely on daily. And when they’re gone, doctors have to use alternatives that may be less effective, more toxic, or harder to dose. The result? More hospitalizations, longer stays, and higher costs. This isn’t just a business problem. It’s a public health emergency.What Resilience Really Means
Resilience doesn’t mean building a wall around U.S. manufacturing. It means having options. The U.S. Department of Health and Human Services defines a resilient supply chain as one that can anticipate, prepare for, respond to, and recover from disruptions while still delivering critical medicines. That’s it. No magic. Just three core abilities: preparation, response, and recovery. Leading companies are already doing this. They map out their supply chains across 12 to 15 tiers of suppliers-not just the main API maker, but the chemical vendor, the packaging supplier, the logistics partner. They ask: What if the port in Mumbai closes? What if a key raw material is embargoed? What if a quality audit fails in Bangalore? Then they build backups. The most effective strategies use three tools: buffer stock, dual sourcing, and regional networks. Buffer stock means keeping 60 to 90 days of inventory for essential drugs. Dual sourcing means having at least two approved suppliers for every critical API. Regional networks mean spreading manufacturing across North America, Europe, and Asia-not just putting everything in one place. This isn’t about nationalism. It’s about risk reduction.The Tech That’s Changing the Game
Old-school batch manufacturing-where drugs are made in large, slow batches-is being replaced by continuous manufacturing. Think of it like a soda fountain instead of a bottle-filling line. The ingredients flow in, the reaction happens in real time, and the finished product comes out continuously. This system cuts facility size by 30-40%, uses 20-25% less energy, and reduces waste by 15-20%. It’s faster, cleaner, and more flexible. But adoption is slow. As of mid-2025, the FDA has approved only 12 continuous manufacturing lines. Over 10,000 batch lines are still in use. Why? Cost. A single continuous manufacturing facility costs $50-150 million. That’s 3 to 5 times more than a traditional plant. But the return comes in speed and reliability. Companies using this tech report 18-22% better yield and 25-30% fewer quality errors. AI is helping too. Machine learning models now predict disruptions 60 to 90 days in advance with 85-90% accuracy. They track weather patterns, port delays, political unrest, and even social media chatter about raw material shortages. One major pharma company reduced its response time to a supplier failure from 45 days to just 7 by integrating AI into its risk dashboard. Blockchain is another quiet hero. It tracks every batch from raw material to patient. Pilots show it cuts counterfeit drugs by 70-75%. That’s not just about safety-it’s about trust. When you know exactly where your medicine came from, you can react faster when something goes wrong.
What the Government Is Doing (And What It’s Not)
The U.S. government is stepping in. In August 2025, an executive order launched the Strategic Active Pharmaceutical Ingredients Reserve. The goal? Stockpile 90 days’ worth of 150 essential medicines by 2027. The government has also pledged $1.2 billion through the CHIPS and Science Act to rebuild domestic manufacturing. Another $800 million is proposed for 2025. But these efforts are only part of the solution. Tariffs won’t fix this. Forcing all manufacturing back to the U.S. is impossible and expensive. The National Academies of Sciences warns that over-relying on domestic suppliers creates new risks-like putting all your eggs in one basket. The real win? A balanced mix: strategic domestic capacity for critical drugs, diversified global sourcing for others, and smart stockpiles for emergencies. The FDA is also speeding things up. New guidance cuts approval times for continuous manufacturing from 24-36 months down to 12-18 months. That’s a game-changer for innovation.Who’s Doing It Right-and Who’s Falling Behind
Big pharma companies with over $10 billion in revenue are leading the charge. Eighty-five percent have full resilience programs. They spend 8-10% of their supply chain budget on preparedness. Mid-sized firms? Only 42%. Small companies? Just 18%. That’s a problem. Smaller firms often supply generics and essential medicines. If they can’t afford resilience, the whole system weakens. The companies winning are those that break down silos. Supply chain teams work with R&D, finance, and regulatory affairs from day one. They run drills-simulating a shutdown in India or a quality failure in Germany. They don’t wait for a crisis to test their plan. They practice it. One medtech company partnered with ZS Associates to rebuild its API sourcing. They mapped every supplier, identified 12 high-risk dependencies, and built dual sources for all critical items. When a fire hit their primary API plant in 2024, they switched to their backup supplier in 72 hours. No shortage. No lost revenue. Just a well-prepared team.The Real Cost of Inaction
Building resilience isn’t cheap. It adds 8-12% to the cost of goods sold. But the cost of doing nothing is higher. ZS Associates found that companies with strong resilience strategies avoid $14.7 million in lost revenue per major disruption. They also see a 1.8x return on investment within three years-not from selling more drugs, but from avoiding chaos. The human cost is even steeper. A shortage of insulin, heparin, or chemotherapy drugs doesn’t just hurt profits. It hurts people. Nurses have to ration. Patients miss treatments. Deaths rise. Resilience isn’t a luxury. It’s a moral obligation.What You Can Do-Even If You’re Not a Pharma Exec
You don’t need to run a billion-dollar company to care about this. If you’re a patient, ask your doctor: Is this drug made in the U.S.? Are there alternatives if it runs out? If you’re a pharmacist, push for dual sourcing with your distributor. If you’re a policymaker, support funding for continuous manufacturing and supply chain mapping tools. The future of medicine won’t be determined by who makes the cheapest pills. It’ll be determined by who can guarantee that the right drug is there when it’s needed most. That’s the new standard. And it’s within reach.What causes most drug shortages today?
Most drug shortages today are caused by disruptions in the global supply of active pharmaceutical ingredients (APIs), especially from China and India. These include factory shutdowns due to quality failures, natural disasters, political tensions, or export restrictions. Even a single supplier failure can trigger a nationwide shortage because many drugs rely on just one or two API sources.
How much inventory should hospitals keep to prevent shortages?
For essential medicines like antibiotics, heart drugs, and anesthetics, hospitals and distributors should maintain 60 to 90 days of inventory. This buffer gives time to switch suppliers or reroute shipments during disruptions. The FDA and CDC recommend this level specifically for drugs with limited or single sources.
Is making drugs in the U.S. the best solution?
Not entirely. While increasing U.S. production helps-especially for critical drugs like sterile injectables-it’s not practical or cost-effective to bring everything home. The best approach is strategic domestic capacity for high-risk medications, combined with diversified global sourcing and strong stockpiles. Relying only on U.S. suppliers creates new single-point failures.
What technologies are helping fix supply chain problems?
Continuous manufacturing, AI-powered risk forecasting, and blockchain traceability are the top three technologies making a difference. Continuous manufacturing cuts costs and speeds production. AI predicts disruptions 60-90 days in advance. Blockchain ensures every batch is trackable, reducing counterfeits and speeding recalls.
Why don’t more companies build resilient supply chains?
Three main barriers: cost, silos, and uncertainty. Building resilience requires $50-150 million for new tech, which small firms can’t afford. Many companies still treat supply chain as a separate department, not a core strategy. And with shifting regulations and unclear government incentives, some wait for others to lead.
How long does it take to build a resilient supply chain?
It’s not a one-time project. A full resilience program takes 12-24 months to fully implement. The first 3-6 months are spent mapping suppliers and identifying risks. Another 2-4 months are used for scenario planning. Investment decisions take 1-3 months. But the real work-training, testing, updating-is ongoing. Companies that treat it as a continuous process outperform those that treat it as a project.



lol why are we even talking about this like it’s a new problem? we’ve been warned for 15 years. the factories in china are still running on fumes and we’re still acting surprised when insulin disappears. 🤦♀️
Let’s be clear: the FDA’s new guidance on continuous manufacturing isn’t ‘streamlining’-it’s a desperate attempt to catch up after 20 years of deregulation and outsourcing. You don’t get to call it innovation when you’re just playing catch-up with technology that’s been around since 2010.
I just had to get my mom’s chemo refill last week and the pharmacist said they were out. Not because it was expensive-because no one had backup stock. We’re not talking about fancy new drugs here. We’re talking about stuff that keeps people alive. This isn’t a supply chain issue. It’s a humanity issue.
The real bottleneck isn’t manufacturing-it’s regulatory. Even if a company builds a dual-sourced API line in Ohio, the FDA takes 18 months to approve it. Meanwhile, the same API from India gets cleared in 4. We need parallel review tracks for critical drugs. Stop treating pharma like it’s a startup needing a pitch deck.
Dual sourcing is table stakes. What’s missing is dynamic inventory allocation. AI can predict disruptions, but if your ERP system can’t auto-redirect shipments based on real-time risk scores, you’re just collecting data. Companies need integrated platforms-not spreadsheets and prayers.
One must question the epistemological foundations of resilience. If a supply chain is designed to ‘recover,’ then recovery implies prior collapse. Is resilience not merely the institutionalization of failure? Perhaps the true solution lies not in redundancy, but in the radical decentralization of pharmaceutical knowledge-putting synthesis in the hands of local pharmacists, not multinational conglomerates.
I get the tech stuff, but what about the people? The workers in those Indian and Chinese factories? They’re not just cogs. If we move production back here, we’re not just saving lives-we’re creating jobs. We just need to pay them enough to stay.
The fact that we’re even having this conversation is a national disgrace. We have the technology. We have the capital. We have the scientific expertise. Yet we let a handful of foreign factories dictate whether a child gets antibiotics or not. This isn’t economics. This is moral cowardice.
I’ve seen this play out in my hospital. We had a shortage of epinephrine last winter. Nurses were cutting vials in half. I get that cost matters, but when you’re staring at a 5-year-old in respiratory arrest and the only thing that can save them is gone? That’s not a supply chain problem. That’s a failure of will.
Let’s be real. The real reason we’re not making drugs here is because the government is in bed with Big Pharma and China. The same people who got us into this mess are now selling us the ‘solution.’ Blockchain? AI? That’s just glitter on a corpse. The real agenda? Control. Surveillance. You think they want you to know where your meds come from? Nah. They want you to just shut up and take the pill.
It is, regrettably, evident that the prevailing discourse on pharmaceutical supply chain resilience remains fundamentally underdeveloped. The reliance upon technological panaceas-continuous manufacturing, AI forecasting, blockchain-distracts from the structural imperative: sovereign capacity for critical API synthesis. One must not conflate efficiency with security.
So we’re spending billions to build factories in the US so we can still import the chemicals from China? That’s not resilience. That’s a tax write-off with a flag on it.
They’re gonna need way more than $1.2B. You think you can build a pharma plant like a Tesla Gigafactory? Nah. These places need HEPA filters, sterile rooms, FDA inspectors on site 24/7. And good luck finding engineers who know how to run them. We’ve been outsourcing the skills for 30 years. You don’t just flip a switch.