Alcohol and Medications – What You Need to Know
If you take prescription or over‑the‑counter meds, mixing them with alcohol can change how the drug works or cause nasty side effects. Knowing which combos are risky helps you avoid surprise symptoms and keep your health on track.
Common Interactions
Many medicines react to alcohol in a similar way: they either get stronger or weaker, or they trigger extra drowsiness. Pain relievers like ibuprofen or acetaminophen can irritate the stomach more when you drink, increasing the chance of ulcers or bleeding. Antibiotics such as metronidazole and tinidazole cause a sudden flushing reaction—think hot face, rapid heartbeat—if you sip wine.
Blood thinners are another big group. Warfarin, for example, works by slowing clot formation; alcohol can swing the effect up or down, making bleeding more likely or reducing protection against clots. Antidepressants and anti‑anxiety meds often make you feel sleepy on their own, so adding a few drinks can leave you too drowsy to drive or work safely.
Even everyday supplements aren’t immune. Vitamin B6 can be broken down faster when you drink heavily, while herbal extracts like St. John’s wort may increase how quickly your liver processes alcohol, leading to lower blood‑alcohol levels but higher strain on the organ.
How to Stay Safe
The easiest rule is: check the label or ask a pharmacist before you have a drink. If the medication says “no alcohol,” stick to it—those warnings are there for a reason. When the label isn’t clear, look up the drug name online or call your doctor.
If you decide to sip, keep the amount low. One standard drink (a 12‑oz beer, 5‑oz wine, or 1.5‑oz spirit) usually won’t cause major problems with most meds, but everyone’s tolerance is different. Pay attention to how you feel; if you notice extra dizziness, nausea, or trouble sleeping, stop drinking and talk to a professional.
Timing matters too. Some drugs stay in your system for days, so even occasional weekend drinks can interact. Try to leave at least 24‑48 hours between taking the medication and having alcohol, especially with antibiotics or blood thinners.
Finally, don’t forget hydration. Alcohol dehydrates you, which can make side effects feel worse. Drink water alongside any alcoholic beverage and eat a balanced meal to slow absorption.
By checking labels, limiting intake, and listening to your body, you can enjoy a drink without messing up your medication plan. Stay informed, stay safe, and keep feeling good.
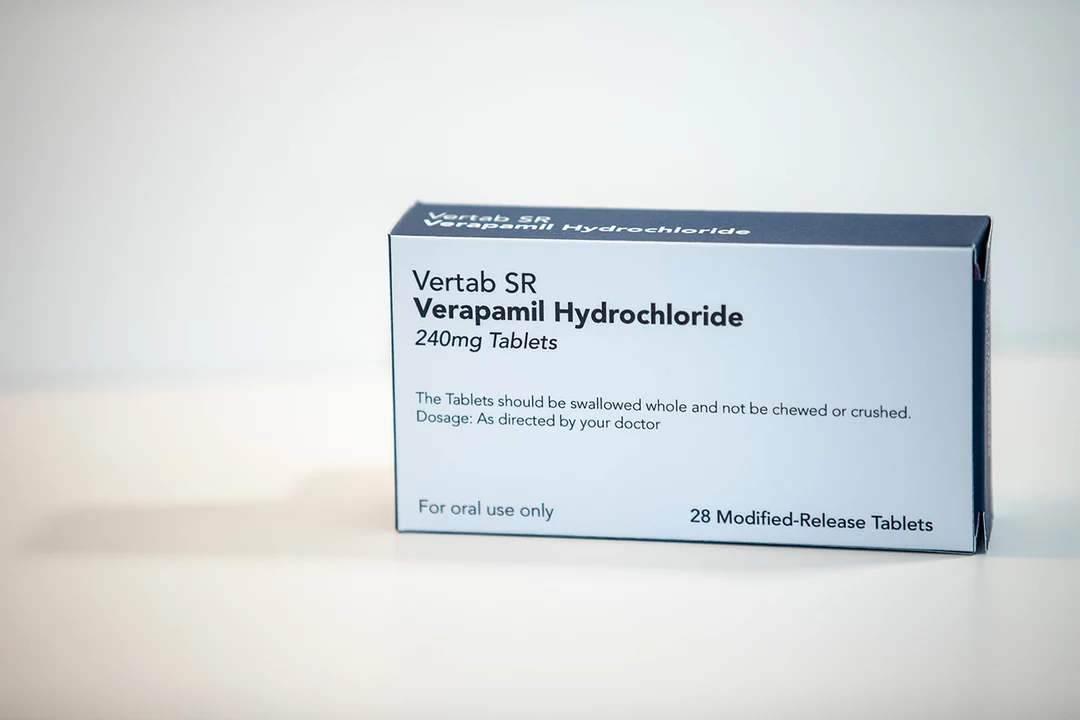
As a blogger, I feel it's important to discuss the risks associated with combining Verapamil and alcohol. Verapamil is a medication used to treat conditions like high blood pressure and chest pain, while alcohol is a widely consumed recreational beverage. Combining these two substances can lead to dangerous side effects such as dizziness, drowsiness, and an increased risk of accidents. Additionally, alcohol may reduce the effectiveness of Verapamil, making it harder to control your symptoms. It's crucial for individuals taking Verapamil to understand these risks and avoid consuming alcohol to ensure their safety and the effectiveness of their medication.