
REM sleep behavior disorder isn’t just about acting out dreams-it’s a warning sign your brain may be changing in ways that could lead to Parkinson’s disease, dementia with Lewy bodies, or another serious neurological condition. People with RBD don’t just kick or yell in their sleep. They might jump out of bed, punch the air, or even fall downstairs trying to escape a dream. These aren’t random accidents. They’re symptoms of a breakdown in the brain’s normal sleep shutdown system. And while the behaviors are scary, the real concern is what’s happening underneath: up to 74% of people with idiopathic RBD will develop a neurodegenerative disease within 12 years.
What Exactly Happens During REM Sleep Behavior Disorder?
Normally, during REM sleep, your brain paralyzes your muscles so you don’t act out your dreams. It’s a protective feature. In RBD, that paralysis fails. Electromyography (EMG) tests show abnormal muscle activity during REM sleep-sometimes in as much as 15% of sleep cycles. This isn’t just twitching. It’s complex, goal-directed movements: throwing punches, screaming, running in place, or even getting up and walking. The average person with RBD has about 4.2 episodes per hour. That’s nearly one every 15 minutes. These behaviors aren’t random. They mirror the content of the dream. Someone dreaming they’re being chased might run. Someone dreaming they’re fighting off an intruder might swing at their partner. The result? Broken bones, bruises, concussions, and fractured relationships. One study found that 78% of patients with RBD made changes to their bedroom to stay safe-removing sharp furniture, padding walls, and storing weapons elsewhere. Even with treatment, 42% eventually sleep separately from their partner just to avoid injury.How Is RBD Diagnosed?
You can’t diagnose RBD from a symptom checklist alone. You need a sleep study-polysomnography (PSG). This is the only way to confirm REM sleep without atonia (RSWA), the hallmark of the disorder. During the test, electrodes track brain waves, eye movements, and muscle tone. If your leg or arm muscles show activity during REM sleep when they should be completely still, that’s RBD. The International Classification of Sleep Disorders (ICSD-3) requires that RSWA be present in at least 15% of REM sleep epochs. But many patients wait years for a diagnosis. Symptoms often start in the 50s or 60s, and doctors may mistake them for nightmares, sleepwalking, or even psychiatric issues. That delay is dangerous. Early detection matters because RBD is one of the strongest predictors of future neurodegeneration.First-Line Medications: Melatonin vs. Clonazepam
There are no FDA-approved drugs specifically for RBD. But two medications are used off-label-and they work for most people. Melatonin is the safer first choice. It’s a natural hormone that helps regulate sleep-wake cycles. For RBD, doctors start with 3 mg at bedtime and slowly increase to 6 mg, then 9 mg, and up to 12 mg if needed. It takes 2 to 4 weeks at each dose to see results. About 65% of patients report fewer or milder episodes. Side effects are mild: maybe a little morning grogginess, or a headache. One 68-year-old man went from seven episodes a week to one after starting 6 mg of melatonin. His only complaint? A brief period of drowsiness that faded after two weeks. Clonazepam works faster and more powerfully. It’s a benzodiazepine that enhances GABA, calming brain activity. Doses start at 0.25 mg to 0.5 mg at night. Most patients respond within days. Studies show 80% to 90% see dramatic improvement. But it comes with risks. About 22% feel dizzy. 18% become unsteady. 15% get excessively sleepy during the day. For older adults, the fall risk jumps by 34%. Some patients develop tolerance. Others struggle with withdrawal-nightmares, agitation, and rebound symptoms can hit if they stop suddenly. One patient quit after three months because he started falling twice a month.
Other Medications and Emerging Options
Not everyone responds to melatonin or clonazepam. For those who don’t, doctors may try other options. Pramipexole, a dopamine agonist used for Parkinson’s and restless legs syndrome, helps about 60% of RBD patients-especially those who also have RLS. Dose ranges from 0.125 mg to 0.5 mg daily. It’s not a first-line choice, but it’s useful when movement symptoms overlap. Rivastigmine, a cholinesterase inhibitor used in Alzheimer’s and dementia, showed promise in one small trial for RBD patients with mild cognitive impairment. It’s not widely used, but it’s an option when other treatments fail. The most exciting development is in dual orexin receptor antagonists. Orexin is a brain chemical that keeps you awake. Blocking it helps you sleep more deeply and quietly. Mount Sinai’s 2023 research showed these drugs reduced dream enactment behaviors by 78% in animal models. Suvorexant (Belsomra), already FDA-approved for insomnia, is being studied for RBD. Neurocrine Biosciences’ drug, NBI-1117568, received Fast Track designation from the FDA in January 2023. Phase II trials are underway, with results expected in mid-2024. This could be the first treatment designed specifically for RBD-not just masking symptoms, but targeting the brain’s sleep-wake control system.Neurological Monitoring: Why It’s Non-Negotiable
Having RBD doesn’t just mean you need better sleep. It means you need regular neurological checkups. The American Academy of Neurology recommends annual exams for anyone diagnosed with idiopathic RBD. Why? Because the risk of developing Parkinson’s, dementia with Lewy bodies, or multiple system atrophy is high-about 6.3% per year. That’s more than 70% over a decade. Early signs might be subtle: a slight tremor, reduced sense of smell, constipation, or changes in voice tone. These aren’t normal aging. They’re red flags. Neurologists look for motor symptoms, cognitive decline, autonomic dysfunction (like blood pressure drops or urinary issues), and changes in sleep architecture. Brain imaging like DaTscan can detect dopamine loss before full Parkinson’s develops. Some centers now use biomarkers in spinal fluid or skin biopsies to detect alpha-synuclein, the abnormal protein linked to these diseases. The goal isn’t to predict the future-it’s to intervene early.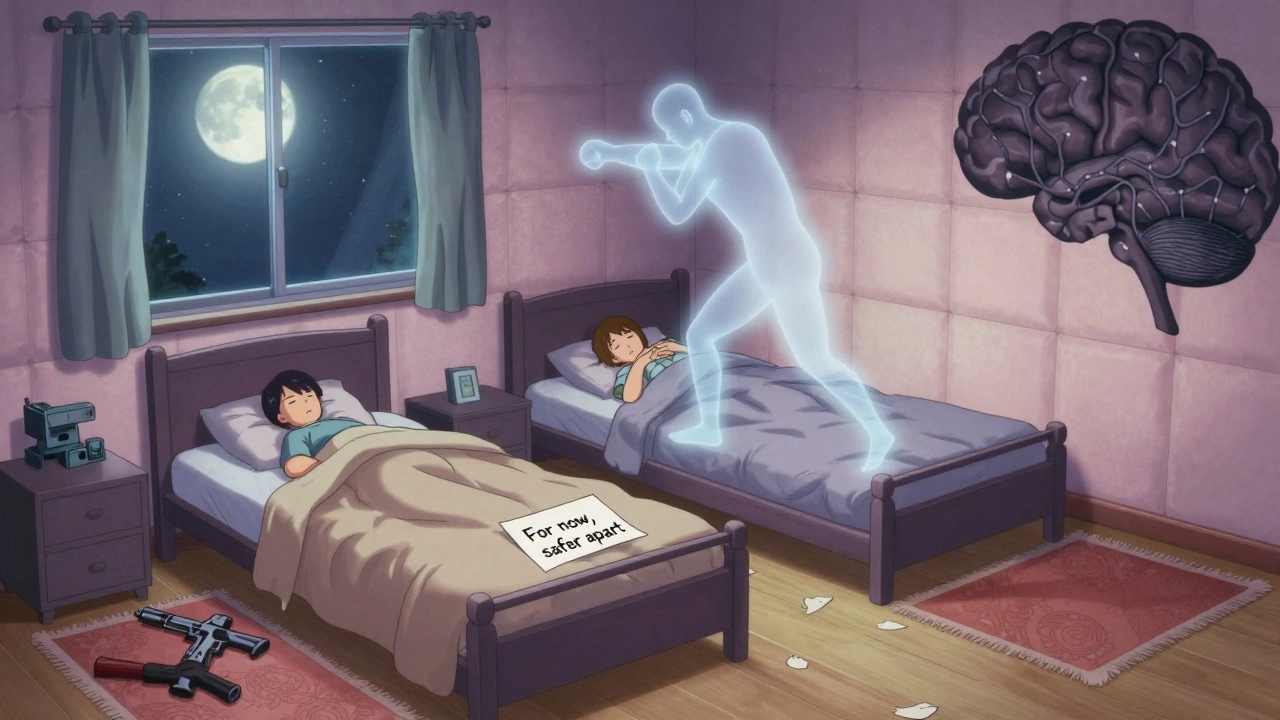
Safety First: Modifying Your Environment
Medication helps. But you still need to make your bedroom safe. The Cleveland Clinic and other experts recommend:- Remove all weapons from the bedroom
- Pad sharp corners of furniture
- Place thick rugs or mats next to the bed
- Install bed rails if you’re at risk of falling
- Consider sleeping in a separate room until symptoms are controlled
What’s Next for RBD Treatment?
Right now, we treat the symptoms. But the real frontier is stopping the disease before it starts. Researchers are exploring whether drugs that target alpha-synuclein-like immunotherapies or gene therapies-can slow or prevent neurodegeneration in RBD patients. Clinical trials are beginning to test this idea. If successful, RBD could become the first condition where we prevent Parkinson’s before it begins. For now, the message is clear: if you or your partner are acting out dreams, don’t ignore it. See a sleep specialist. Get a polysomnogram. Start treatment. Make your room safe. And get neurological follow-up. This isn’t just about better sleep. It’s about protecting your brain for the years ahead.Can REM sleep behavior disorder be cured?
There’s no cure for RBD yet. Current treatments like melatonin and clonazepam reduce symptoms in most patients, but they don’t stop the underlying brain changes. RBD is often an early sign of neurodegenerative diseases like Parkinson’s or dementia with Lewy bodies. Research is now focused on finding treatments that can delay or prevent these diseases from developing.
Is RBD a sign of Parkinson’s disease?
Yes, in many cases. About 73.5% of people with idiopathic RBD develop a neurodegenerative synucleinopathy-most commonly Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy-within 12 years. RBD often appears years or even decades before motor symptoms like tremors or stiffness. It’s one of the strongest known predictors of these diseases.
How does melatonin help with RBD?
Melatonin helps restore the brain’s natural muscle inhibition during REM sleep. It’s a hormone that regulates sleep cycles and may enhance the brain’s ability to suppress movement during dreaming. Doses of 3 to 12 mg at bedtime reduce dream enactment behaviors in about 65% of patients. It’s preferred for older adults and those with other health conditions because it has fewer side effects than clonazepam.
Why is clonazepam effective but risky for RBD?
Clonazepam works by boosting GABA, a calming neurotransmitter that suppresses muscle activity during sleep. It’s effective in 80-90% of cases and often works within days. But it’s a benzodiazepine, which can cause dizziness, unsteadiness, daytime sleepiness, and memory issues. In older adults, it increases fall risk by 34%. Long-term use can lead to dependence or withdrawal symptoms like nightmares and agitation if stopped suddenly.
Can alcohol make RBD worse?
Yes. Even one or two alcoholic drinks can trigger or worsen RBD episodes in 65% of patients. Alcohol disrupts REM sleep and reduces the brain’s ability to maintain muscle paralysis during dreaming. Avoiding alcohol is one of the most important non-medication steps for managing RBD safely.
What should I do if I suspect I have RBD?
Talk to your doctor and ask for a referral to a sleep specialist. Keep a sleep diary noting any dream enactment, injuries, or partner complaints. Record any other symptoms like loss of smell, constipation, or stiffness. A polysomnography sleep study is required for diagnosis. In the meantime, make your bedroom safer: remove weapons, pad sharp furniture, and avoid alcohol.
Are there new drugs being developed for RBD?
Yes. Dual orexin receptor antagonists like suvorexant and Neurocrine Biosciences’ NBI-1117568 are in clinical trials. These drugs target the brain’s wakefulness system and have shown up to 78% reduction in dream enactment in animal studies. The FDA granted Fast Track status to NBI-1117568 in early 2023, meaning approval could come faster. These represent the first potential treatments designed specifically for RBD, not just repurposed from other conditions.



Let’s be real-this isn’t medicine, it’s a slow-motion neurological car crash waiting to happen. 74% of people with RBD develop Parkinson’s or Lewy body dementia? That’s not a disorder, that’s a death sentence with a sleep mask. And melatonin? A sugar pill with a side of delusion. Clonazepam’s the only thing that works, and yes, it’s risky-but so is letting your brain rot unchecked.
Okay, but have you considered that this isn’t just a neurological glitch-it’s a symptom of modern life? EMG readings, sleep studies, dopamine agonists… all just Band-Aids on a system that’s been poisoned by EMFs, glyphosate, and the silent war waged by Big Pharma to keep us docile. They don’t want you to know that RBD is your body screaming that your pineal gland is calcifying from fluoride in the water. Melatonin’s a placebo because the real cure-detoxing your environment-isn’t patentable. I’ve seen people reverse it with red light therapy, grounding mats, and eliminating all processed foods. The doctors won’t tell you this because they’re paid by the pharma lobby.
And don’t get me started on clonazepam. Benzodiazepines? That’s just chemical repression. Your brain isn’t broken-it’s awakened. And they’re terrified of what happens when people stop sleeping like zombies.
Stop overcomplicating this. Melatonin works for some. Clonazepam works better. Alcohol makes it worse. Sleep in another room. End of story.
Really appreciate the breakdown on the meds. I’ve seen a few patients in my clinic go from seven episodes a week to near-zero on 9mg melatonin-no dizziness, no dependency. It’s not sexy, but it’s safe. Clonazepam’s like using a flamethrower to light a candle. Works great until you burn the house down. And yeah, the 34% fall risk in older adults? That’s not a number-it’s a grandmother on the ER floor.
Also, the orexin antagonists? That’s the future. If NBI-1117568 pans out, we might actually be looking at disease modification, not just symptom suppression. That’s huge.
Consciousness is a fragile illusion. Sleep is the veil. When it tears, we see the machinery.
Just had a 67-year-old patient on 12mg melatonin for 8 months. No more punching the air. No more broken nightstand. He said his wife cried the first time she slept through the night in 11 years. That’s the real win here-not the EMG data, not the DaTscan. It’s the quiet.
And yeah, avoiding alcohol? Non-negotiable. One glass of wine and it’s like flipping a switch. The brain’s inhibition is already compromised-alcohol just yanks the last safety latch.
So… let me get this straight. You’re telling me that acting out dreams is a sign of impending Parkinson’s? And we’re just going to give people more drugs? What about the fact that this has been linked to childhood trauma, spiritual awakening, and ancestral memory? No one talks about the metaphysical angle. You’re all just chasing biomarkers while ignoring the soul. And don’t even get me started on how the DSM ignores the spiritual component of sleep disorders. This is medical reductionism at its worst.
Big picture: RBD is the canary in the coal mine for synucleinopathies. The fact that we can detect alpha-synuclein in skin biopsies now? That’s game-changing. We’re moving from reactive to predictive neurology. The real win isn’t melatonin-it’s early intervention. If we can slow or halt neurodegeneration before motor symptoms appear, we’re talking about preventing Parkinson’s before it starts. That’s not hype. That’s Phase III trial data.
Also, the orexin antagonists? Suvorexant’s already FDA-approved for insomnia. Repurposing it for RBD is low-hanging fruit. NBI-1117568 could be the first disease-modifying therapy for RBD. This isn’t just sleep medicine anymore-it’s neuroprotection.
If you or someone you love is acting out dreams-don’t wait. Don’t dismiss it as ‘just bad dreams.’ Get the sleep study. Start the melatonin. Make the room safe. This isn’t about being dramatic-it’s about protecting the people you care about. I’ve seen families fall apart because no one took it seriously. Then the falls happen. Then the diagnosis comes. Then the grief. You don’t have to wait for tragedy to act. Small steps now save lives later.
You’re not alone. There are support groups. There are neurologists who specialize in this. There’s hope. And yes-it’s scary. But you’re stronger than the fear.
My dad had RBD. Took him 7 years to get diagnosed. By then, he was already showing early tremors. We padded the room, switched to melatonin, cut out alcohol-life got quieter. He’s 76 now, still driving, still reading poetry before bed. I’m not saying it’s easy. But it’s manageable. And honestly? The fact that we’re even talking about disease-modifying treatments now? That’s progress. Thank you for writing this.
Wait, so you’re telling me I can’t have my nightly whiskey because my brain’s gonna turn into a dementia factory? Cool. Cool cool cool. So what’s next? No caffeine? No sex? No laughing too hard? Next you’ll tell me I have to stop breathing during REM sleep. This is just another way for doctors to sell you pills and make you paranoid about your own dreams. I’m sleeping in my clothes with a baseball bat now. Thanks for the reassurance.
The clinical data presented here is accurate and well-sourced. It is imperative that individuals exhibiting REM sleep behavior disorder seek evaluation by a board-certified sleep specialist. Pharmacological interventions, environmental modifications, and longitudinal neurological monitoring are evidence-based best practices. Avoidance of alcohol is strongly supported by the literature. This condition warrants neither alarmism nor dismissal.