
Glaucoma Medication Selector
Recommended Medications
Detailed Comparison
When doctors prescribe eye drops for glaucoma, the choice isn’t always clear‑cut. Betoptic comparison often lands on the table because Betaxolol is a well‑known beta‑blocker, but dozens of other drops claim similar pressure‑lowering power with different side‑effect profiles.
What is Betoptic (Betaxolol)?
Betoptic is the brand name for betaxolol hydrochloride, a selective beta‑1 adrenergic blocker formulated as a 0.5% ophthalmic solution. It was introduced in the early 1990s and quickly became a staple for primary open‑angle glaucoma (POAG) and ocular hypertension.
Betaxolol works by reducing the production of aqueous humor, the fluid that fills the front part of the eye. Less fluid means lower intraocular pressure (IOP), which is the main driver of optic‑nerve damage in glaucoma.
Who typically uses Betoptic?
Patients diagnosed with POAG, especially those who also have cardiovascular concerns, are often steered toward Betoptic because its beta‑1 selectivity spares beta‑2 receptors in the lungs. This makes it a safer bet for people with mild asthma or chronic obstructive pulmonary disease (COPD).
However, the drug isn’t without drawbacks. Common complaints include transient eye irritation, a bitter taste after instillation, and occasional systemic effects like bradycardia.
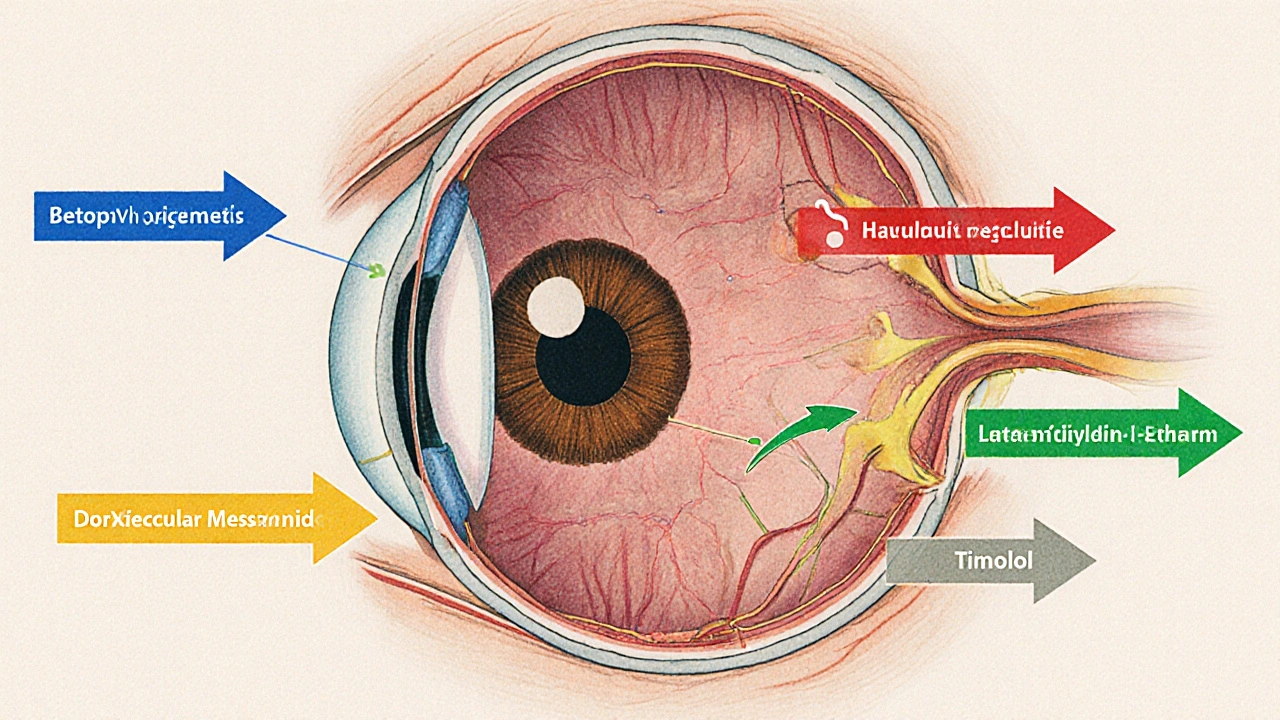
Major Alternatives on the Market
Below is a quick snapshot of the most frequently prescribed glaucoma drops that sit next to Betoptic in a doctor’s toolbox.
- Timolol - a non‑selective beta‑blocker (0.5% solution) that has been a workhorse for decades.
- Latanoprost - a prostaglandin analogue (0.005% solution) celebrated for once‑daily dosing.
- Brimonidine - an alpha‑2 agonist (0.2% solution) that also offers neuroprotective benefits.
- Dorzolamide - a carbonic anhydrase inhibitor (2% solution) that reduces fluid production via a different enzyme pathway.
All of these agents treat the same condition-elevated IOP-but they differ in mechanism, dosing frequency, side‑effects, and cost.
How These Drugs Compare
| Drug | Class | Typical Dose | IOP Reduction (average) | Common Side‑effects | Special Considerations |
|---|---|---|---|---|---|
| Betoptic | Selective beta‑1 blocker | One drop BID | ≈22% | Eye irritation, bitter taste, occasional bradycardia | Safer for mild asthma; avoid in severe COPD |
| Timolol | Non‑selective beta‑blocker | One drop BID | ≈23% | Bronchospasm risk, systemic fatigue | Contraindicated in asthma/COPD |
| Latanoprost | Prostaglandin analogue | One drop QHS | ≈30% | Eye redness, darkening of iris, eyelash growth | Preferred for once‑daily adherence; not for pregnant women |
| Brimonidine | Alpha‑2 agonist | One drop TID | ≈20% | Dry eye, fatigue, allergic‑type reactions | Neuroprotective claims; avoid in severe renal disease |
| Dorzolamide | Carbonic anhydrase inhibitor | One drop BID | ≈18% | Metallic taste, eye discomfort | Useful in combination therapy; watch for sulfa allergy |
Pros and Cons of Betoptic Compared to Its Rivals
Advantages of Betoptic
- Beta‑1 selectivity lowers the risk of bronchospasm, making it a safer choice for patients with mild asthma.
- Proven efficacy-clinical trials from the 1990s still show a reliable 20‑25% drop in IOP.
- Relatively inexpensive generic version is widely available.
Drawbacks of Betoptic
- Requires twice‑daily dosing, which can hurt adherence compared with once‑daily prostaglandins.
- Systemic absorption can cause mild heart‑rate slowing, so patients on cardio‑active meds need monitoring.
- Some users report a persistent bitter taste that lasts minutes after instillation.
How the alternatives stack up
- Timolol is slightly more potent but carries a higher bronchospasm risk-bad news for anyone with respiratory disease.
- Latanoprost delivers the deepest IOP reduction with only one nightly drop, but it can change eye color and cause eyelash growth that some find cosmetic, others love.
- Brimonidine offers a neuroprotective edge, yet its three‑times‑daily schedule and dry‑eye side‑effects can be a turn‑off.
- Dorzolamide works via a distinct enzyme pathway, useful when beta‑blockers fail, but it can cause a metallic taste and isn’t suitable for sulfa‑allergic patients.
Choosing the Right Medication for Your Situation
Doctors usually run through a short decision matrix before writing a prescription. Here’s a simplified version you can review with your eye‑care professional:
- Respiratory health: If you have asthma or COPD, favor Betoptic over Timolol.
- Adherence potential: If you struggle with twice‑daily dosing, Latanoprost’s nightly drop may be a better fit.
- Cosmetic concerns: Want to avoid iris darkening or eyelash changes? Skip prostaglandins.
- Allergy profile: Sulfa‑allergic patients should steer clear of Dorzolamide.
- Cost considerations: Generic Betoptic and Timolol are typically the cheapest; branded prostaglandins can be pricier.
Ultimately, the “best” drug is the one you’ll actually use consistently. Bring up any side‑effects you notice early-doctors can switch you to another class without jeopardizing vision.
Monitoring and Follow‑Up
Regardless of the chosen drop, regular IOP checks are a must. Most ophthalmologists recommend re‑checking pressure 4-6 weeks after starting a new medication, then every 3-4 months once stable. In addition to pressure readings, visual‑field testing helps catch subtle nerve‑fiber loss before it becomes obvious.
If your IOP isn’t dropping by at least 15‑20% after a month, your doctor may add a second drug (often a carbonic anhydrase inhibitor) or consider laser therapy.
Frequently Asked Questions
Can I use Betoptic if I have high blood pressure?
Yes, in most cases. Betaxolol’s beta‑1 selectivity means it has minimal impact on blood‑pressure control, but your physician should monitor both IOP and blood‑pressure during the first few weeks.
How fast does Betoptic start working?
You’ll usually see a measurable drop in IOP within 30‑60 minutes after the first dose, with the peak effect around 4‑6 hours.
Is it safe to combine Betoptic with Latanoprost?
Combination therapy is common when a single drug can’t achieve target pressure. Because the two drugs work via different mechanisms, they’re generally safe together, but your doctor will watch for additive side‑effects like ocular redness.
What should I do if I miss a dose of Betoptic?
Take the missed dose as soon as you remember, unless it’s almost time for your next scheduled dose. In that case, skip the missed one-don’t double up.
Are there any natural alternatives to Betoptic?
Lifestyle changes-like regular exercise, a diet rich in leafy greens, and proper hydration-can support eye health, but they don’t replace prescription drops for IOP control. Always discuss any supplement use with your eye doctor.
Can pregnant women use Betoptic?
Beta‑blockers are generally classified as Category C. If you’re pregnant or planning a pregnancy, talk to your ophthalmologist about safer alternatives like certain prostaglandin analogues.
Choosing between Betoptic and its alternatives isn’t a one‑size‑fits‑all decision. By weighing respiratory health, dosing convenience, side‑effect tolerance, and cost, you can land on the eye‑drop that keeps your vision safe and your routine simple.



When evaluating Betoptic against its peers, the beta‑1 selectivity is a clinically meaningful distinction that mitigates bronchospasm risk in patients with mild reactive airway disease. The drug’s efficacy, hovering around a 22 % IOP reduction, aligns with the historical benchmarks set by non‑selective beta‑blockers while offering a slightly better safety margin. Cost considerations also favor Betoptic, as the generic formulation is widely available and typically less expensive than prostaglandin analogues. Nonetheless, the twice‑daily dosing schedule can erode adherence, especially when patients are already juggling multiple ophthalmic agents. For clinicians, balancing respiratory comorbidities, adherence potential, and systemic cardiovascular effects remains the cornerstone of personalized therapy.
Betoptic offers a solid middle ground for most glaucoma patients.
The pharmacodynamic profile of betaxolol reveals a high affinity for β1‑adrenergic receptors, thereby attenuating aqueous humor production via cAMP modulation.
The selectivity translates into a reduced incidence of bronchoconstrictive events compared with pan‑β antagonists such as timolol.
Moreover, the ocular bioavailability of the 0.5 % solution is facilitated by corneal permeation enhancers that bypass the conjunctival epithelium.
Clinical trial data from the early 1990s demonstrate a mean intraocular pressure (IOP) decrement of 22 % after a two‑week titration period.
Subsequent meta‑analyses confirm that this effect size remains statistically non‑inferior to that of newer prostaglandin analogues when adherence is accounted for.
However, systemic absorption through nasolacrimal drainage can precipitate bradycardic episodes in patients with pre‑existing sinus node dysfunction.
The bitter taste reported by a subset of users is attributable to residual drug in the nasolacrimal sac, a phenomenon mitigated by punctal occlusion techniques.
From a cost‑effectiveness standpoint, the generic formulation of betaxolol exhibits a favorable incremental cost‑utility ratio relative to brand‑only agents.
In patients with comorbid mild asthma, the drug’s β1 specificity offers a therapeutic window absent in non‑selective beta‑blockers, aligning with the American Academy of Ophthalmology’s recommendation for pulmonary‑sparing agents.
Nevertheless, the BID dosing frequency imposes a logistical burden that can degrade real‑world adherence, as evidenced by pharmacy refill adherence metrics.
Combination therapy with a carbonic anhydrase inhibitor is a viable escalation strategy, leveraging synergistic mechanisms of aqueous humor suppression.
The ocular surface tolerance profile remains acceptable, with transient conjunctival hyperemia resolving within 48 hours in the majority of cases.
Patients should be counseled on the importance of proper drop instillation technique to minimize systemic exposure.
Ongoing monitoring of heart rate and blood pressure is prudent during the initiation phase, especially in polypharmacy contexts.
Ultimately, the decision matrix for Betoptic should integrate respiratory status, adherence propensity, and financial considerations to optimize individualized care.
Oh, the drama of choosing eye drops! Imagine the night‑time ritual, a single drop of latanoprost dancing on the cornea like a glittery ballerina, only to leave your iris forever tinted like a midnight sky. Yet Betoptic waltzes in, twice a day, with that lingering bitter after‑taste that haunts the palate like a bad breakup. The cost‑factor? Betoptic is the humble workhorse, while its glam cousins demand a king’s ransom. If you’ve ever wrestled with a three‑times‑daily schedule, you’ll know the existential dread that follows. But behold, the beta‑1 selectivity, a subtle hero in the saga of respiratory safety. In the grand theatre of glaucoma therapy, each drug claims a starring role, and the audience-your eyes-just wants a calm ending. So, pick your potion, dear reader, and may your pressure stay low and your lashes stay normal.
While the preceding analysis is exhaustive, it falls prey to an overreliance on dated trial data, neglecting the pharmacogenomic nuances that modern ophthalmology now embraces. The assertion that systemic absorption is merely “mitigated” overlooks recent findings on cytochrome‑mediated metabolism. A truly elite appraisal would integrate these variables rather than resting on generic cost‑effectiveness arguments.
Philosophically, the selection of a medication is a microcosm of the broader human endeavor to balance risk and reward. Each drop embodies a trade‑off, a negotiated compromise between ocular pressure and systemic wellbeing. In that light, adherence emerges not merely as a behavior but as an ethical commitment to one’s own visual future. Therefore, the clinician’s role transcends prescription; it becomes a conduit for personal responsibility. Ultimately, vision preservation is as much a moral imperative as a clinical goal.
Betoptic works fine but the twice‑daily hassle is stupid.
Actually, the proper term is “twice‑daily,” not “twice daily,” and “hassle” could be replaced with “adherence challenge” for precision. Maintaining grammatical consistency helps readers trust the information. Great point though, the dosing frequency is a key factor.
The phrase “once‑daily dosing” should be hyphenated, and “prostaglandin analogues” is the correct spelling in American English. Minor edits improve clarity.
Oh wow, thank you for that groundbreaking insight that Betoptic is…a “solid middle ground.” I’m sure no one ever thought of that before. Maybe next you’ll tell us water is wet.