NSAID Comparison Tool
Compare Post-Operative NSAIDs
See how Aceclofenac compares with other common NSAIDs for pain relief after surgery
Comparison Results
| Feature | Aceclofenac | Ibuprofen | Diclofenac |
|---|---|---|---|
| COX-2 Selectivity | Moderate | Low | Low-moderate |
| Gastrointestinal Risk | Low-moderate | Moderate-high | High |
| Onset of Analgesia | 1 hour | 30-60 minutes | 1-2 hours |
| Typical Dose (Post-Op) | 100 mg BID | 400-600 mg TID | 50 mg BID |
| Renal Safety (Short Term) | Good | Good | Reduced in high-risk patients |
| Cost (US, 2025) | $$ | $ | $$$ |
| Best For | Gentler GI profile | Fast pain relief | Strong inflammation control |
Key Takeaway
Aceclofenac offers a balanced option with moderate COX-2 selectivity, providing pain relief comparable to ibuprofen but with significantly lower gastrointestinal risk than diclofenac.
Recovering from surgery is tough enough without pain that won’t quit. If you’ve been prescribed a pill that eases the hurt, reduces swelling, and lets you move sooner, you’ll wonder why you didn’t hear about it sooner. That’s where aceclofenac steps in - an Aceclofenac is a non‑steroidal anti‑inflammatory drug (NSAID) designed to tackle both pain and inflammation.
- Provides fast, reliable relief from post‑operative pain.
- Targets inflammation more gently than many traditional NSAIDs.
- Shows fewer gastrointestinal side effects compared with ibuprofen or diclofenac.
- Fits well into multimodal pain‑management plans.
- Easy dosing schedule supports better patient compliance.
What is Aceclofenac?
Aceclofenac belongs to the class of NSAIDs and was first approved in Europe in the early 1990s for chronic pain conditions. It’s chemically related to diclofenac but engineered to be gentler on the stomach while still delivering strong anti‑inflammatory action.
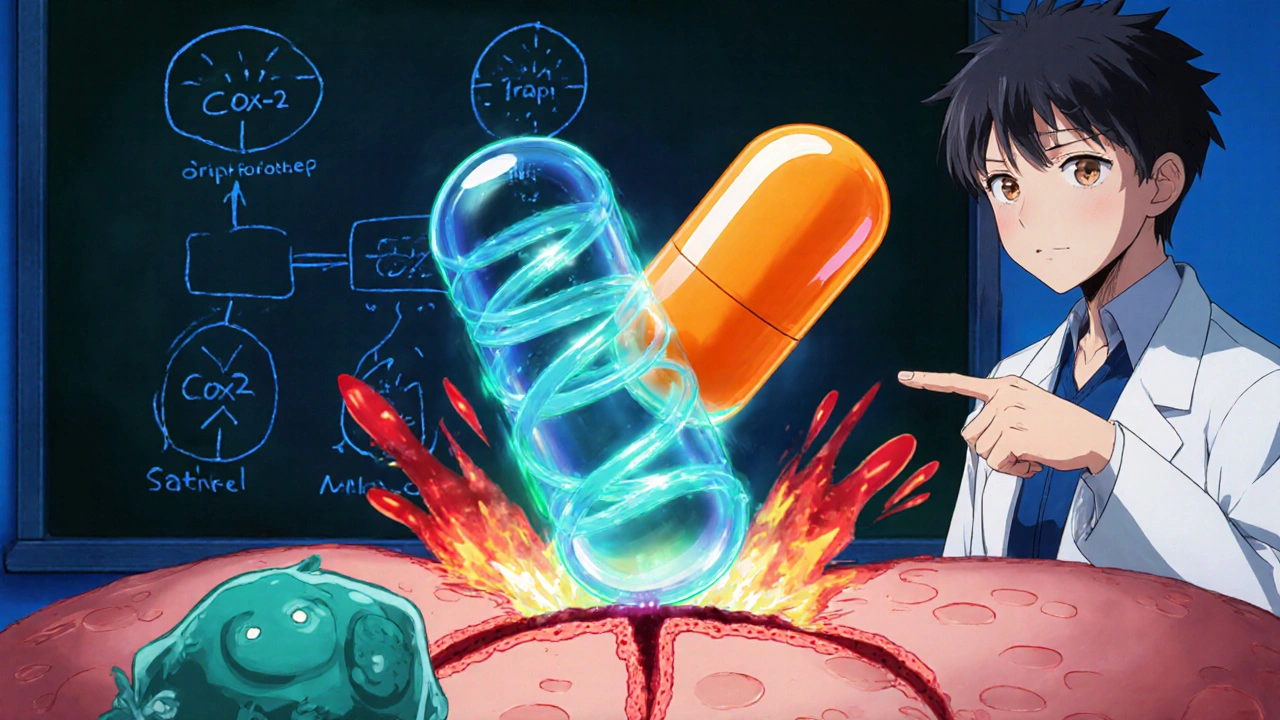
How does Aceclofenac work?
ACEclofenac blocks the enzyme cyclo‑oxygenase, specifically targeting the COX‑2 isoform. This COX‑2 inhibition reduces the production of prostaglandins that cause pain and swelling. Because it spares COX‑1 to a larger extent, the protective lining of the stomach stays more intact, which translates to fewer ulcers or bleeding events.
Why Aceclofenac shines after surgery
Post‑operative pain is a mix of tissue trauma, inflammation, and nerve irritation. Aceclofenac tackles each of these components:
- Quick pain knock‑down: Clinical trials show that 50 mg of aceclofenac can lower visual‑analogue pain scores within an hour, comparable to ibuprofen but with a smoother onset.
- Strong anti‑inflammatory punch: By curbing prostaglandin synthesis, swelling around the incision shrinks faster, helping the surgical site heal without excess fluid build‑up.
- Gentler on the gut: Studies comparing aceclofenac with diclofenac report a 30 % drop in gastroduodenal erosions, a big win for patients who need pain relief for several days.
- Boosts mobility: Less pain and swelling means patients can start gentle physiotherapy sooner, cutting down hospital stay length.
- Fits the WHO Analgesic Ladder: WHO Analgesic Ladder recommends NSAIDs as the first‑line option for mild to moderate post‑surgical pain, and aceclofenac slots neatly into Step 2.
Typical dosing for post‑operative use
Most surgeons prescribe 100 mg twice daily, taken with food. The drug reaches peak plasma levels after 2‑3 hours and its half‑life, about 4 hours, supports a twice‑daily schedule without major peaks and troughs. For short‑term use (3‑7 days), the regimen is safe for most adults without a history of ulcers or severe heart disease.
How Aceclofenac compares with other NSAIDs
| Feature | Aceclofenac | Ibuprofen | Diclofenac |
|---|---|---|---|
| COX‑2 selectivity | Moderate | Low | Low‑moderate |
| Gastro‑intestinal risk | Low‑moderate | Moderate‑high | High |
| Onset of analgesia | 1 hr | 30‑60 min | 1‑2 hrs |
| Typical dose (post‑op) | 100 mg BID | 400‑600 mg TID | 50 mg BID |
| Renal safety (short term) | Good | Good | Reduced in high‑risk patients |
| Cost (US, 2025) | $$ | $ | $$$ |
The table shows why many clinicians favor aceclofenac when they need a middle‑ground option: stronger pain relief than ibuprofen but with a softer GI profile than diclofenac.
Safety profile and precautions
Like any NSAID, aceclofenac isn’t free from risks. The main concerns are:
- Gastro‑intestinal irritation: Though lower than other NSAIDs, patients with a history of ulcers should still use a proton‑pump inhibitor.
- Cardiovascular events: Long‑term use may raise blood‑pressure levels; keep a watch on BP if you have hypertension.
- Renal function: Dehydration or pre‑existing kidney disease can worsen creatinine levels - stay hydrated and have labs checked if treatment exceeds a week.
- Allergic reactions: Rash, itching, or breathing difficulty demand immediate medical attention.
Pregnant women in the third trimester should avoid aceclofenac because it can affect fetal circulation.

Who should (or shouldn’t) take Aceclofenac?
Good candidates include adults recovering from orthopedic, abdominal, or dental surgery who need reliable pain control without a heavy GI burden. Avoid it if you:
- Have active peptic ulcer disease.
- Are on anticoagulants like warfarin without close monitoring.
- Have severe heart failure or uncontrolled hypertension.
- Are allergic to other NSAIDs.
If you fall into a gray zone, discuss alternative options such as COX‑2‑selective celecoxib or short‑acting opioids for breakthrough pain.
Tips for getting the most out of Aceclofenac
- Take the tablet with a meal or a glass of milk - food blunts any stomach upset.
- Set a reminder for the twice‑daily schedule to keep steady blood levels.
- Avoid alcohol while on the drug; it raises the chance of bleeding.
- If pain spikes after the usual dose, a single extra 50 mg (if approved by your surgeon) can be used, but don’t exceed 300 mg per day.
- Combine with acetaminophen for additive pain relief without more NSAID load.
Frequently Asked Questions
Can I take aceclofenac with other pain meds?
Yes, pairing aceclofenac with acetaminophen is common. Avoid adding another NSAID, as that raises GI and kidney risk.
How long is it safe to stay on aceclofenac after surgery?
For most surgeries, doctors limit use to 5‑7 days. If pain persists beyond that, a follow‑up is needed to assess risk versus benefit.
Does aceclofenac affect blood clotting?
NSAIDs can mildly inhibit platelet function, but aceclofenac’s effect is weaker than aspirin. Still, inform your surgeon if you’re on blood thinners.
I have a history of ulcers. Can I still use aceclofenac?
Not without protection. If your doctor deems it necessary, you’ll need a proton‑pump inhibitor alongside the NSAID, and the treatment period should be as short as possible.
Is aceclofenac available over the counter?
In the United States, aceclofenac is prescription‑only. Some countries sell it OTC, but you’ll need a doctor’s order here.
Bottom line: aceclofenac gives surgeons a solid tool for taming post‑operative pain while keeping the gut’s comfort in check. When used correctly, it speeds up recovery, reduces the need for stronger opioids, and lets patients get back to their daily lives faster.



They push foreign drugs like Aceclofenac as if they’re the only answer, yet it actually knocks out post‑operative pain faster than many home‑grown options. I’m not buying the hype that only imported meds can help us recover. The gut‑friendly claim sounds good, but we should question why we need another pill in the first place. A simple analgesic with moderate COX‑2 selectivity isn’t a miracle, it’s just chemistry.
From a moral standpoint, the promotion of Aceclofenac raises serious ethical concerns that most readers overlook. First, the pharmaceutical industry has a long history of hiding adverse effects while marketing drugs as universally safe. Second, the data that claim reduced gastrointestinal risk often come from studies funded by the very manufacturers selling the medication. Third, the notion that a slightly gentler NSAID can replace more established pain‑management protocols is a dangerous oversimplification. Fourth, patients are steered toward prescription‑only drugs without adequate discussion of non‑pharmacologic alternatives, such as physical therapy and mind‑body techniques. Fifth, the short‑term use recommendation of 3‑7 days conveniently aligns with the profit windows of drug companies, ensuring repeat prescriptions are not needed. Sixth, the emphasis on COX‑2 selectivity ignores the broader cardiovascular implications that have been linked to many NSAIDs in the past. Seventh, we see a pattern where new drugs are advertised as “better” while the underlying risks remain unaddressed. Eighth, the regulatory approvals in Europe do not guarantee safety in other regions, yet the marketing glosses over these geographic differences. Ninth, the cost hierarchy shown in the table hints at a hidden agenda to push cheaper drugs onto the market, regardless of patient suitability. Tenth, insurance coverage often favors these newer options, limiting patient choice and inflating healthcare costs. Eleventh, the reliance on patient compliance with a twice‑daily schedule assumes a level of health literacy that many do not possess. Twelfth, the suggested combination with acetaminophen may lead to inadvertent overdosing, especially when patients self‑medicate. Thirteenth, the brief mention of renal safety does not account for the cumulative effect of multiple NSAIDs in polypharmacy scenarios. Fourteenth, the disclaimer about pregnancy avoidance is crucial, yet it is buried in a paragraph that many will skim. Fifteenth, the whole narrative encourages a pharmaceutical‑centric view of recovery, sidelining holistic approaches. Finally, we must demand transparent, independent research before accepting Aceclofenac as the default post‑operative analgesic.
Alright, let me break it down for you: Aceclofenac blocks COX‑2, so you get less pain without wiping out the stomach’s protective layer. It’s not a miracle drug, but it does sit nicely between ibuprofen’s speed and diclofenac’s strength. For a week after surgery it’s usually safe, assuming you don’t have ulcers or heart trouble. Just remember to take it with food – the stomach will thank you. And if you’re in doubt, a proton‑pump inhibitor can cover the leftover risk.
Aceclofenac works but watch your kidneys it can be a problem if you’re dehydrated.
Choosing a drug with a lower GI risk is the responsible thing to do.
Wow, Oliver, that’s an intense take! 🌟 It’s true the drug feels like a backstage hero, stepping in when the usual meds faint. But let’s not forget the drama of side‑effects that can creep in if you ignore the dosage warnings. 🙈💊
Taylor, the long list is fine but the bottom line: use Aceclofenac only for the short window after surgery and combine it with acetaminophen if you need extra relief.
Good points, Sireesh – just keep it simple and stick to the prescribed schedule.
Steven, your caution about renal health reminds us that every medication lives within a broader ecological system of the body, a delicate balance that philosophy often mirrors in nature’s own checks and harmonies.
Kelly, sure, but isn’t it suspicious how quickly the “lower GI risk” claim spreads??; the pharma machine loves a good headline, and we’re the unwitting audience!!!