
Antidepressant Weight Gain Comparison Tool
Compare the weight gain risks of common antidepressants. Based on clinical studies showing average weight changes over 6 and 24 months.
Filter by Risk Level
Antidepressant Weight Gain Comparison
| Medication | 6-Month Gain | 24-Month Gain | Weight Risk |
|---|---|---|---|
| Wellbutrin (Bupropion) | -0.25 lbs | +1.2 lbs | Low Risk |
| Cymbalta (Duloxetine) | +1.2 lbs | +1.7 lbs | Moderate Risk |
| Paxil (Paroxetine) | +1.4 lbs | +2.9 lbs | High Risk |
| Lexapro (Escitalopram) | +1.4 lbs | +3.6 lbs | Moderate Risk |
| Zoloft (Sertraline) | +0.5 lbs | +3.2 lbs | Moderate Risk |
| Remeron (Mirtazapine) | +2.5 lbs | +5-7 lbs | High Risk |
| Elavil (Amitriptyline) | +2.0 lbs | +6-8 lbs | High Risk |
What This Means For You
If you're on a high-risk medication:
Consider discussing with your doctor about switching to a lower-risk option like bupropion. The first 6 months are critical - weight gain often starts after 3-6 months and becomes more significant after 1 year.
If you're on a moderate-risk medication:
These medications cause moderate weight gain over time. You can manage this with lifestyle changes and possibly adding metformin or GLP-1 agonists as recommended by your doctor.
If you're on a low-risk medication:
Bupropion is the exception. It often causes slight weight loss in the first 6 months and minimal weight gain over 2 years. This is due to its unique mechanism affecting norepinephrine and dopamine rather than serotonin.
Action Steps
Don't stop your medication due to weight gain alone. Talk to your doctor about:
- Switching to a lower-risk antidepressant
- Adding metformin or GLP-1 agonists to manage weight
- Implementing lifestyle changes (protein-rich meals, regular movement)
- Tracking your weight and diet
- Checking your CYP2C19 status if you're a slow metabolizer
Remember: Weight gain isn't always caused by the medication itself. Sometimes it's your body responding to improved mood and increased appetite as depression lifts.
When you start taking an antidepressant, you’re hoping to feel better - less overwhelmed, more in control, maybe even like yourself again. But for many people, one of the unexpected side effects is something they didn’t sign up for: weight gain. It’s not just about clothes feeling tighter. For some, it’s a slow, steady climb that shakes their confidence, disrupts their health, and even makes them quit their medication. The truth? About 55-65% of people on long-term antidepressants gain weight. And it’s not random - certain drugs are far more likely to cause it than others.
Why Do Antidepressants Make You Gain Weight?
It’s not as simple as “the drug makes you hungry.” The science behind this is layered. Antidepressants change how your brain handles serotonin, dopamine, and other chemicals that control mood, appetite, and energy use. In the first few weeks, some people actually lose weight because their appetite drops or they feel less urge to binge-eat. But after six months to a year, something shifts. The brain adapts. Serotonin receptors slow down. That triggers cravings - especially for carbs and sugary snacks. Your body also starts storing fat more easily. Insulin sensitivity drops. Leptin and ghrelin, the hormones that tell you when you’re full or hungry, get out of sync. Some drugs, like tricyclics and mirtazapine, also block histamine receptors. That’s why people on these meds often feel sleepy and crave snacks - it’s a direct effect on your brain’s reward and hunger centers. And it’s not just about the drug. Your genes matter too. If you’re a slow metabolizer of certain antidepressants (thanks to your CYP2C19 gene), you’re more likely to build up higher levels in your system, which increases the risk.Which Antidepressants Are Most Likely to Cause Weight Gain?
Not all antidepressants are created equal when it comes to weight. Some are nearly neutral. Others? They’re practically known for it.- High-risk: Amitriptyline, nortriptyline, imipramine (TCAs), mirtazapine (Remeron), paroxetine (Paxil), phenelzine (Nardil)
- Moderate-risk: Citalopram (Celexa), escitalopram (Lexapro), sertraline (Zoloft), duloxetine (Cymbalta)
- Lowest risk: Bupropion (Wellbutrin)
| Medication | Weight Gain at 6 Months | Weight Gain at 24 Months |
|---|---|---|
| Bupropion (Wellbutrin) | -0.25 lbs | +1.2 lbs |
| Duloxetine (Cymbalta) | +1.2 lbs | +1.7 lbs |
| Paroxetine (Paxil) | +1.4 lbs | +2.9 lbs |
| Escitalopram (Lexapro) | +1.4 lbs | +3.6 lbs |
| Sertraline (Zoloft) | +0.5 lbs | +3.2 lbs |
| Mirtazapine (Remeron) | +2.5 lbs | +5-7 lbs |
| Amitriptyline (Elavil) | +2.0 lbs | +6-8 lbs |
Why Bupropion Is the Exception
Bupropion works differently. Instead of targeting serotonin, it boosts norepinephrine and dopamine. These chemicals are linked to energy, focus, and appetite suppression. That’s why people on bupropion often report feeling less hungry and more motivated to move. In the first six months, most lose a little weight. Even after two years, the gain is minimal - barely over a pound. It’s not a magic bullet (some people still gain), but it’s the best option if weight is a major concern. And yes - it works for depression. Studies show it’s as effective as SSRIs for many people. It’s also used for smoking cessation, which tells you something about its impact on cravings. If your doctor hasn’t mentioned it, ask. It’s not always the first choice, but it should be on the table.
It’s Not Always the Drug - Depression Itself Changes Your Body
Before you blame the medication, consider this: maybe you’re not gaining weight - maybe you’re regaining it. Many people start antidepressants after months (or years) of depression. Depression can crush your appetite. You stop eating. Or you eat junk food because it’s easy. You lose muscle. Your metabolism slows. When the meds kick in, your mood lifts - and so does your appetite. Suddenly, you’re hungry again. You start cooking. You eat more. You gain weight. But it’s not because the drug made you fat. It’s because you’re healing. This is why weight gain on antidepressants is so hard to pin down. Sometimes it’s the drug. Sometimes it’s recovery. Often, it’s both. That’s why experts say: don’t stop your meds because you’re gaining weight. Talk to your doctor. Adjust the plan. Don’t quit.How to Manage Weight Gain Without Stopping Your Antidepressant
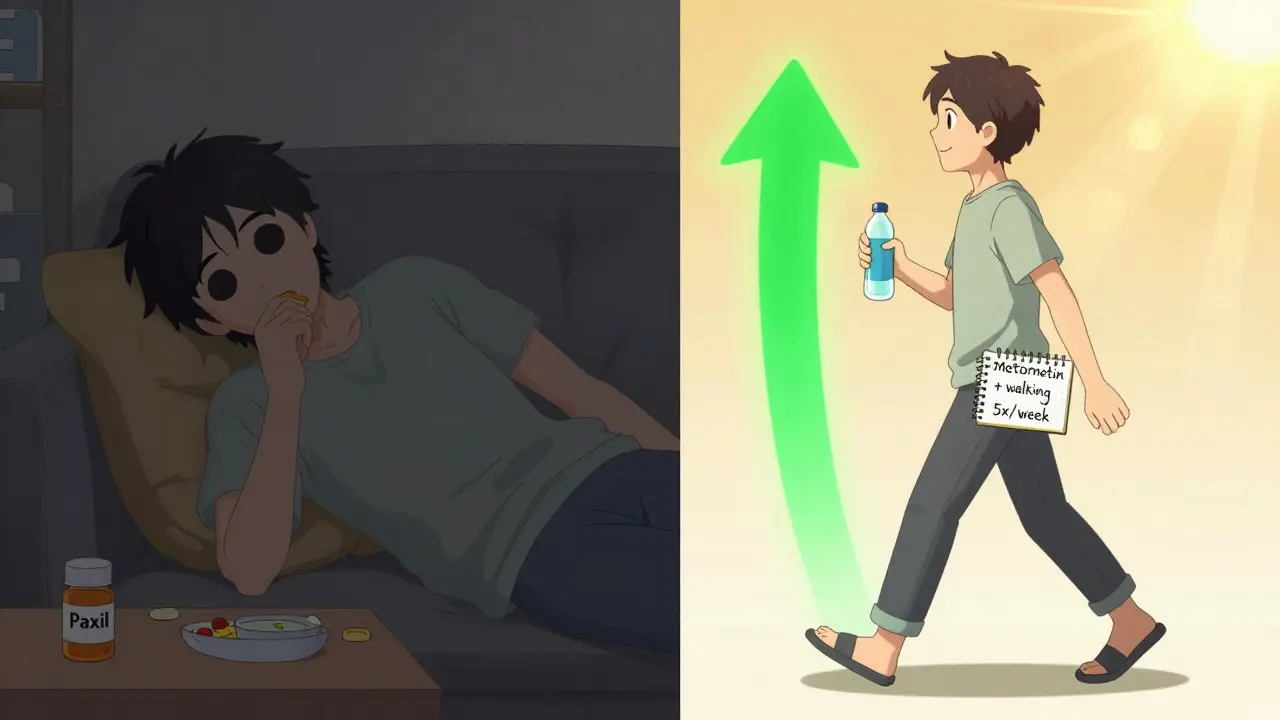
You don’t have to choose between mental health and your waistline. Here’s what actually works:- Switch meds. If you’re on paroxetine or mirtazapine and gaining weight, ask about switching to bupropion or sertraline. Studies show switching can stop or reverse the trend. Don’t do it alone - taper under medical supervision.
- Add metformin. This diabetes drug helps your body use insulin better. It’s been shown in trials to cut weight gain by 30-50% in people taking antidepressants. It’s safe, cheap, and often covered by insurance.
- Try GLP-1 agonists. Drugs like semaglutide (Wegovy) or liraglutide (Saxenda) are now being studied for this exact problem. Early results show 5-7% weight loss in people on antidepressants. It’s not FDA-approved for this yet, but many doctors are prescribing it off-label with good results.
- Move more - consistently. You don’t need to run marathons. Just 30 minutes of walking, cycling, or strength training five days a week can offset the metabolic slowdown. Muscle burns more calories than fat - even at rest.
- Watch your carbs. If your brain is craving sugar, don’t fight it - replace it. Swap white bread for whole grain. Choose fruit over candy. Eat protein and fiber first at meals. It slows digestion and keeps blood sugar steady.
What to Do If You’re Already Gaining Weight
If you’ve been on your current antidepressant for over a year and noticed a steady climb on the scale, here’s your action plan:- Track your weight for 4 weeks. Is it steady? Rising? Dropping? This gives you baseline data.
- Review your diet. Are you eating more snacks? More carbs? More late-night meals? Keep a food journal for a week.
- Ask your doctor about your CYP2C19 status. A simple genetic test can show if you metabolize your drug slowly - a major risk factor.
- Request a metabolic panel. Check your fasting glucose, insulin, and triglycerides. If they’re rising, it’s not just fat - it’s early metabolic dysfunction.
- Bring up bupropion, metformin, or a switch to a lower-risk SSRI. Don’t be afraid to ask. This is a common issue - your doctor has seen it before.
When to Consider Stopping - And When Not To
Some people quit their antidepressants because of weight gain. Bad idea. Studies show that stopping increases your chance of depression returning by 30-50%. And once depression comes back, your appetite and energy crash again. It’s a cycle that’s hard to break. The goal isn’t to avoid weight gain at all costs. It’s to manage it while keeping your mental health stable. If your depression is under control and you’re gaining 1-2 pounds a year? That’s manageable. If you’re gaining 10 pounds in 12 months? That’s a red flag. Talk to your provider. There are solutions. You don’t have to live with the side effects.What’s Next? The Future of Antidepressants
Researchers are working on new antidepressants designed to avoid weight gain entirely. Some are targeting specific serotonin receptors that don’t trigger hunger. Others are combining antidepressants with drugs that block histamine or boost metabolism. And the big picture? Scientists are now asking: could the rise in antidepressant use be contributing to the obesity epidemic? One study found that people who took antidepressants and then switched to a high-fat diet gained far more weight than those who only ate poorly. Even after stopping the meds, their bodies held onto the extra fat. That suggests these drugs may cause long-term changes in how your body stores energy - changes that stick around. That’s why managing this side effect isn’t just about looking better. It’s about preventing diabetes, heart disease, and long-term health collapse.Do all antidepressants cause weight gain?
No. While many do, some - especially bupropion - are linked to little or no weight gain, and even modest weight loss in the short term. The risk varies widely by drug class. Tricyclics and mirtazapine carry the highest risk, while SSRIs like sertraline and escitalopram cause moderate gain over time. Bupropion remains the outlier with the lowest impact.
How long does it take to gain weight on antidepressants?
Weight gain usually starts after 3-6 months and becomes more noticeable after a year. Early on, some people lose weight due to reduced appetite. But as the brain adjusts to higher serotonin levels, receptors become less sensitive, triggering cravings and slower metabolism. Most weight gain happens between 6 and 24 months.
Can I lose weight while on antidepressants?
Yes - but it takes effort. Switching to bupropion helps. Adding metformin or GLP-1 agonists can reverse gain. Lifestyle changes - especially protein-rich meals, regular movement, and avoiding processed carbs - are essential. You can’t rely on the drug alone. But with the right combo, weight loss is possible even while staying on treatment.
Is weight gain from antidepressants permanent?
Not always, but it can be. Some people lose the weight after switching meds or stopping. Others retain the extra fat because the drugs may cause lasting changes in how the body stores energy. Research suggests that long-term use - especially combined with poor diet - can rewire metabolic pathways. That’s why early intervention matters more than waiting until you’ve gained 20 pounds.
Should I stop my antidepressant if I’m gaining weight?
No - unless your doctor advises it. Stopping abruptly can trigger a return of depression, anxiety, or even suicidal thoughts. Weight gain is a side effect. Depression is a life-threatening illness. Talk to your provider about alternatives: switching meds, adding metformin, or adjusting your diet and activity level. Don’t quit without a plan.



Comments
Post Comment