Alpha-Glucosidase Inhibitors: How They Control Blood Sugar and What You Need to Know
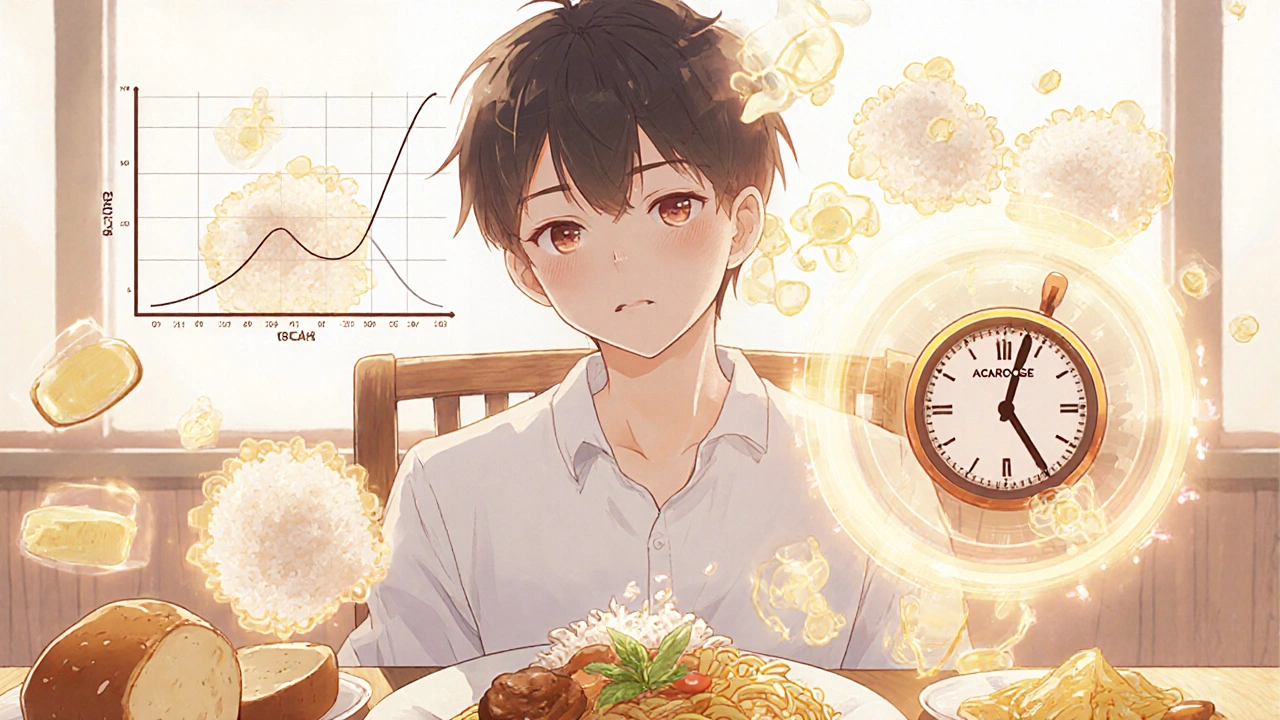
When you eat carbs, your body breaks them down into glucose—and if that happens too fast, your blood sugar spikes. Alpha-glucosidase inhibitors, a class of oral diabetes medications that delay carbohydrate digestion in the small intestine. Also known as carb blockers, they don’t lower insulin or make your body more sensitive to it. Instead, they slow down the enzymes that turn starches and sugars into glucose, so sugar enters your bloodstream gradually. This makes them especially useful for people whose blood sugar shoots up after meals—something common in type 2 diabetes.
These drugs work right in your gut, not in your liver or pancreas. That means they’re less likely to cause low blood sugar on their own, unlike some other diabetes pills. But they’re not magic. They only help with the carbs you eat. If you skip a meal or eat mostly protein and fat, they won’t do much. And because they slow digestion, they often cause bloating, gas, or diarrhea—especially at first. Most people get used to it, but if the side effects are too rough, your doctor might switch you to something else.
They’re not first-line drugs like metformin, but they’re still used—especially in places where people eat a lot of rice, pasta, or bread. In Asia, for example, alpha-glucosidase inhibitors like acarbose and miglitol are more common because diets are higher in complex carbs. They also work well when combined with other meds. If you’re on metformin but still see big spikes after lunch, adding one of these can help smooth things out. And unlike some newer diabetes drugs, they don’t cause weight gain. In fact, some people lose a little weight because they feel full faster or have less appetite after meals.
What you won’t find in the package insert is how real people use them. Some take them right before each meal, others forget and take them with the first bite. Some swear by them; others ditch them after a week of stomach trouble. The key is timing: they need to be taken with the first bite of food to work. If you take them too early or too late, they won’t slow digestion properly. And they won’t help if you eat candy or soda—those sugars are absorbed too fast for these drugs to block.
There’s also a quiet benefit: because they flatten out glucose spikes, they may reduce long-term damage to blood vessels and nerves. That’s not their main job, but it’s why some doctors still recommend them, even with newer options available. They’re cheap, stable, and don’t interact with most other meds—unlike some diabetes drugs that clash with antibiotics or heart medications.
Below, you’ll find real-world guides on how these drugs fit into daily life—what to eat with them, how to handle side effects, how they compare to other treatments, and what to watch for when mixing them with other pills. Whether you’re just starting out or you’ve been on them for years, there’s something here that can help you use them better—and maybe even feel better while doing it.
Precose (acarbose) slows carb digestion but doesn't help with weight or heart health. Learn how metformin, GLP-1 agonists, and SGLT2 inhibitors offer better results for managing type 2 diabetes.