GI Bleeding Risk Assessment Tool
How to Use This Tool
Enter your information to assess your risk of gastrointestinal bleeding when taking SSRIs and NSAIDs together.
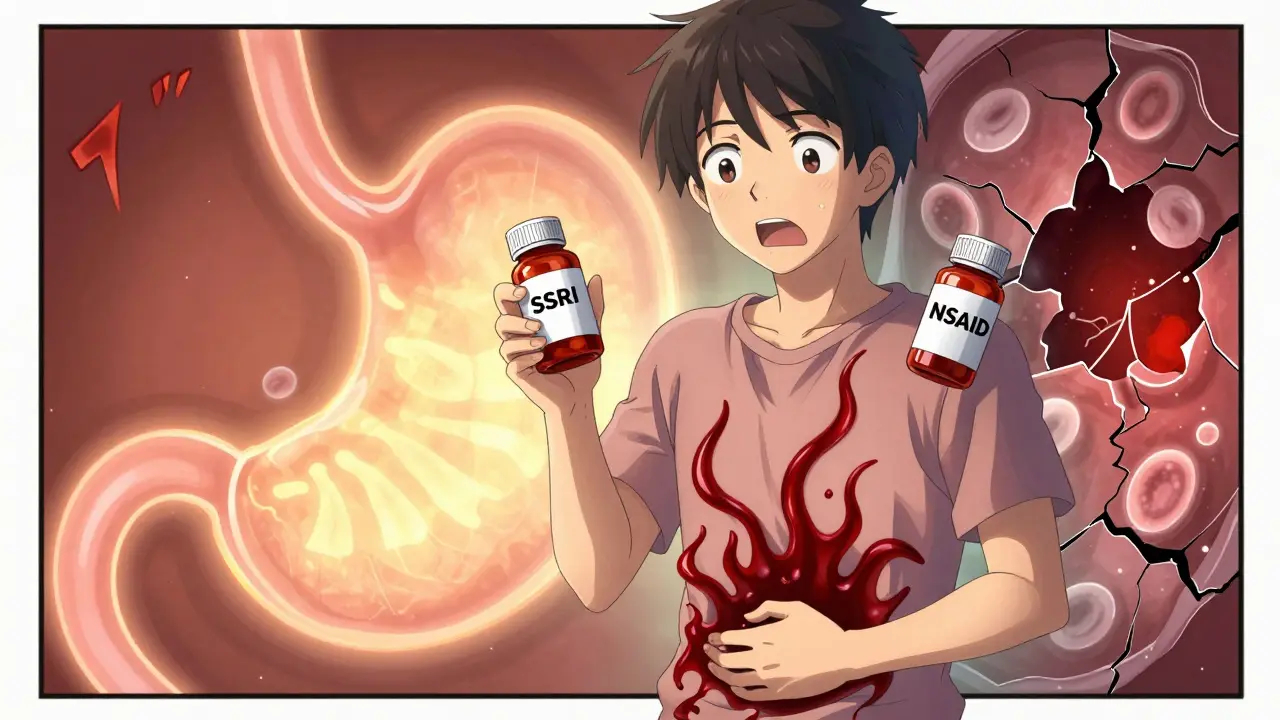
Every year, millions of Americans take SSRIs for depression or anxiety, and just as many reach for NSAIDs like ibuprofen or naproxen for back pain, arthritis, or headaches. But what most people don’t know is that taking these two types of medications together can dramatically increase your risk of a life-threatening bleed in your stomach or intestines. This isn’t a rare side effect. It’s a well-documented, clinically significant interaction that’s happening far too often - and too many doctors and patients are unaware of it.
Why This Combination Is Dangerous
SSRIs - drugs like sertraline, fluoxetine, and citalopram - work by boosting serotonin in the brain to improve mood. But serotonin isn’t just a brain chemical. It’s also critical for blood clotting. Platelets, the cells that stop bleeding, rely on serotonin to stick together and form clots when a blood vessel is damaged. SSRIs block serotonin from being taken back up into platelets, leaving them less able to do their job. The result? Slower, weaker clotting - even if you just scrape your knee. NSAIDs, on the other hand, attack the stomach lining. They shut down COX-1 enzymes, which are responsible for making protective prostaglandins. These prostaglandins keep the stomach’s mucus layer thick, maintain blood flow to the lining, and help repair tiny injuries before they turn into ulcers. When NSAIDs block them, your stomach becomes vulnerable. Even a short course can cause microscopic damage. Long-term use? That’s a recipe for ulcers. Put them together, and you get a one-two punch: your blood can’t clot well, and your stomach lining is already weakened. The risk isn’t just doubled or tripled - it jumps by 75%. That’s not a small number. It means if 100 people take both drugs, about 15 more will have a serious GI bleed compared to those taking just one or neither. And the numbers get worse with age, prior ulcers, or other medications like aspirin or blood thinners.Not All SSRIs or NSAIDs Are Created Equal
Some SSRIs carry slightly higher bleeding risks than others, but the difference is small. Fluvoxamine and paroxetine may have marginally stronger effects on platelets, while escitalopram and sertraline are often considered slightly safer - though still risky when combined with NSAIDs. The key point: all SSRIs affect platelets. There’s no “safe” SSRI if you’re also taking an NSAID. With NSAIDs, the risk varies more clearly. Non-selective NSAIDs like naproxen and diclofenac are the worst offenders. They hit COX-1 hard and cause the most stomach damage. Ibuprofen is a bit gentler, especially at low doses (200-400 mg), but it’s still risky over time. Then there’s celecoxib - a COX-2 selective NSAID. It doesn’t mess with the stomach’s protective prostaglandins nearly as much. Studies show it has a GI bleeding risk close to that of a placebo (odds ratio of 1.16), making it the safest NSAID option when you absolutely need one.Who’s Most at Risk?
This isn’t a problem that affects everyone equally. Certain people are walking into a high-risk situation without even knowing it:- People over 65 - aging stomachs heal slower, and platelet function declines naturally.
- Those with a past history of ulcers or GI bleeding - even if it was years ago.
- Anyone taking low-dose aspirin - it adds another layer of antiplatelet effect.
- Patients on blood thinners like warfarin or apixaban - combining these with SSRIs and NSAIDs can be deadly.
- People with H. pylori infection - this bacteria causes ulcers and makes the stomach even more vulnerable.
What You Can Do: Prevention Is Simple - If You Know How
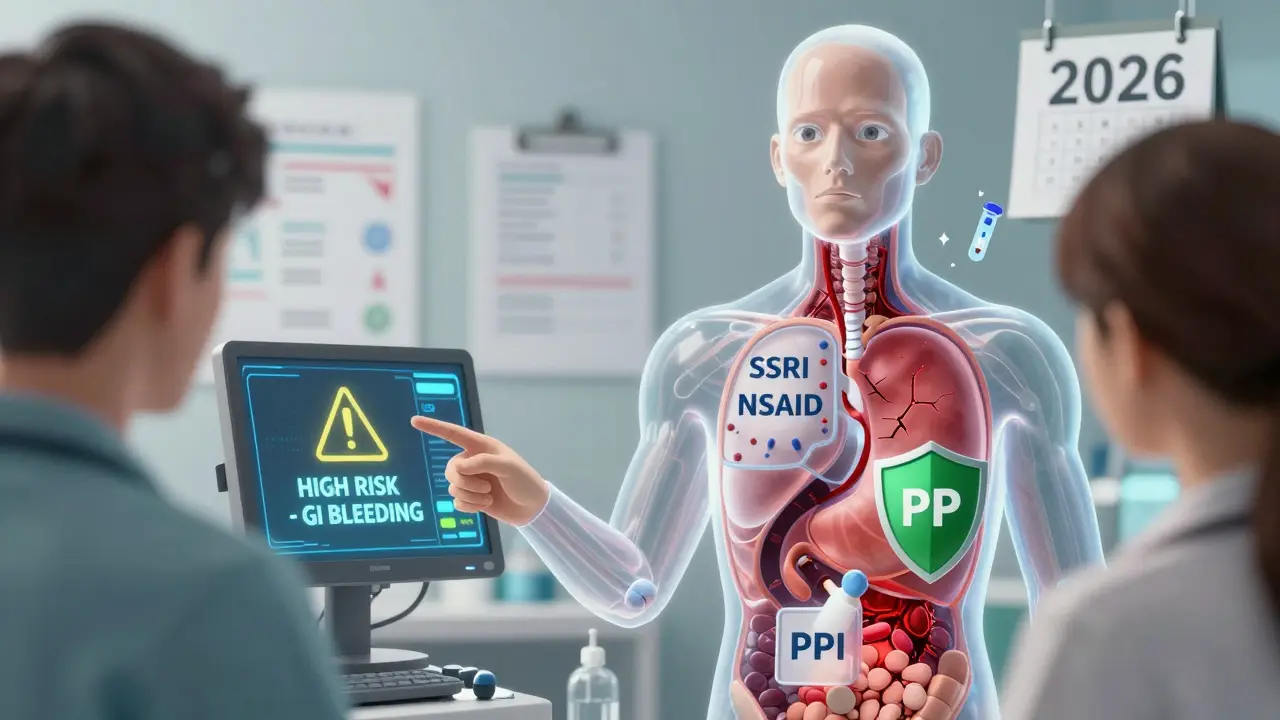
The good news? This risk is almost entirely preventable. You don’t have to choose between managing your pain and your mental health. You just need to make smarter choices. Step 1: Ask if you really need the NSAID. For many types of pain - especially muscle aches, headaches, or mild arthritis - acetaminophen (Tylenol) works just as well without the bleeding risk. It doesn’t affect platelets or the stomach lining. If you’re taking NSAIDs daily for chronic pain, talk to your doctor about alternatives. Physical therapy, heat therapy, or even low-dose antidepressants like duloxetine (which also treats nerve pain) might be better long-term options. Step 2: If you must take an NSAID, pick celecoxib. It’s not perfect - it can raise blood pressure and heart risk in some people - but for GI safety, it’s the clear winner. If celecoxib isn’t right for you, use the lowest effective dose of ibuprofen for the shortest time possible. Never take more than 1,200 mg of ibuprofen per day without medical supervision. Step 3: If you’re on both an SSRI and an NSAID, get a PPI. Proton pump inhibitors like omeprazole (Prilosec), esomeprazole (Nexium), or pantoprazole (Protonix) reduce stomach acid and help the lining heal. Taking a daily 20 mg dose of omeprazole cuts the bleeding risk from this combo by about 70%. That’s not a small win - it brings your risk back down to near-normal levels. And yes, it’s safe for long-term use in most people. The myth that PPIs cause serious long-term harm has been greatly exaggerated. For someone on both SSRIs and NSAIDs, the benefits far outweigh the risks.What Doctors Should Be Doing
A 2021 survey of 1,200 primary care doctors found that fewer than 40% routinely checked for this interaction. That’s unacceptable. This isn’t some obscure drug interaction - it’s one of the most common and dangerous combinations in primary care. Hospitals like Cleveland Clinic and Mayo Clinic have already fixed this by building automated alerts into their electronic health records. When a doctor tries to prescribe an SSRI and an NSAID together, the system pops up a warning: “High risk of GI bleeding. Consider PPI or alternative pain management.” Since 2020, Cleveland Clinic reported a 42% drop in GI bleeding hospitalizations among patients on both drugs - simply because the system forced the issue. Doctors should be using the ACG Upper GI Risk Calculator - a free, evidence-based tool that factors in age, ulcer history, H. pylori status, and other meds - to determine who needs protection. And they should be talking to patients, not just prescribing. If you’re on an SSRI and your doctor gives you ibuprofen for your knee pain, ask: “Is this safe? Should I be on a stomach protector?”
Real Stories, Real Consequences
On Reddit, users describe waking up with black, tarry stools - a classic sign of internal bleeding - and rushing to the ER. One person wrote: “I took sertraline for depression and ibuprofen for my back. I didn’t think it was a big deal. Three days later, I was vomiting blood. I spent a week in the hospital.” But there are also success stories. A woman with rheumatoid arthritis and depression switched from naproxen to celecoxib, started taking omeprazole daily, and kept her sertraline. She’s been symptom-free for over a year. “My doctor finally listened,” she said. “I wish I’d known sooner.” The difference? Awareness. Action. Prevention.What’s Changing in 2026
New research is making prevention even smarter. Scientists are now looking at genetic testing - specifically, CYP2C19 gene variants - to predict who metabolizes PPIs slowly (and thus gets better protection) or who’s more likely to have bad reactions. Some companies are testing pills that combine NSAIDs with built-in PPIs, so you get protection in one tablet. The American College of Gastroenterology is expected to release updated guidelines in early 2024 that will strongly recommend testing for H. pylori before starting dual therapy. If you’re infected, eradicating the bacteria cuts your bleeding risk in half. And AI is stepping in. A new algorithm, trained on millions of health records, can now predict your personal bleeding risk with 86% accuracy - just by looking at your age, meds, lab results, and past medical history. It’s not in every doctor’s office yet, but it’s coming.Bottom Line: Don’t Guess. Ask.
You don’t need to stop your SSRI. You don’t need to suffer through pain. You just need to make sure you’re not putting yourself at unnecessary risk. If you’re taking both an SSRI and an NSAID:- Ask your doctor if you can switch to acetaminophen instead.
- If you need an NSAID, ask if celecoxib is an option.
- Ask if you should be on a daily PPI like omeprazole.
- Ask if you’ve ever been tested for H. pylori.
- Ask for a copy of your risk assessment - don’t just take the prescription and walk out.
Can I take ibuprofen with sertraline?
You can, but it’s not safe without protection. Taking ibuprofen and sertraline together increases your risk of stomach bleeding by about 75%. If you must take both, you should also take a proton pump inhibitor like omeprazole daily. Consider switching to acetaminophen for pain relief instead - it doesn’t carry this risk.
Is celecoxib safer than ibuprofen with SSRIs?
Yes. Celecoxib is significantly safer for your stomach than ibuprofen or naproxen when taken with SSRIs. It doesn’t block the protective prostaglandins in your stomach lining the way non-selective NSAIDs do. Studies show its bleeding risk is close to normal, while ibuprofen still carries a 2-4 times higher risk than placebo. Always discuss with your doctor whether celecoxib is appropriate for your condition.
Do all SSRIs increase bleeding risk equally?
Most SSRIs affect platelet function similarly because they all block serotonin reuptake. Some studies suggest escitalopram or sertraline may be slightly less potent in this effect than fluvoxamine or paroxetine, but the difference is small. No SSRI is considered safe to combine with NSAIDs without protection. The key is not which SSRI you’re on - it’s whether you’re also taking an NSAID.
How long should I take a PPI if I’m on both an SSRI and NSAID?
If you’re on both medications long-term, you should take a proton pump inhibitor daily as long as you’re taking the NSAID. If you stop the NSAID, you can usually stop the PPI after a week or two. For people with prior ulcers or high risk, doctors may recommend continuing the PPI indefinitely. Always follow your doctor’s advice - PPIs are safe for long-term use in this context.
Can I take aspirin with an SSRI and NSAID?
No - this combination is extremely dangerous. Aspirin is itself an NSAID and also interferes with platelet function. Taking aspirin with an SSRI and another NSAID multiplies the bleeding risk even further. If you’re on low-dose aspirin for heart protection, talk to your doctor before starting an SSRI. You may need a PPI and possibly a different pain reliever. Never combine these three without medical supervision.
What are the warning signs of a GI bleed?
Watch for black, tarry stools (melena), vomiting blood (which may look like coffee grounds), sudden dizziness, weakness, or abdominal pain. These are not normal. If you’re on an SSRI and NSAID and notice any of these, go to the ER immediately. GI bleeds can be fatal if not treated quickly.


Wow. Finally someone who gets it. Most docs just shrug and say 'it's fine' while you're slowly bleeding out. I took sertraline + ibuprofen for 8 months. Woke up one morning with black poop. ER. 2 units of blood. No one warned me. Not my PCP, not my psych, not even the pharmacist. This post is a public service.
The data is clear. Combining SSRIs and NSAIDs increases GI bleed risk by 75%. Celecoxib with PPI reduces it by 70%. Acetaminophen is the default choice for mild pain. No ambiguity. Stop guessing. Start acting.
This is just the tip. Big Pharma knows this. They don't warn you because PPIs are more profitable than your life. The real scandal? The FDA has known since 2006. Why no black box warning? Because they're too busy approving new antidepressants with 17 new side effects. Wake up.
PPIs cause kidney failure and dementia lmao. You're trading one problem for two. Just stop taking the SSRI. Your 'depression' is just weak willpower. Pain? You're weak. Stop being a baby. Take ibuprofen. God will protect you.
I mean... it's not just the pharmacology, right? It's the existential loneliness of being a human in a mechanized healthcare system where you're a data point, not a person. The SSRIs are trying to patch the emotional void, the NSAIDs are trying to patch the physical decay, and the PPIs are just... a band-aid on a hemorrhage. We're all just trying to survive a system that doesn't care if we live or die, as long as the billing codes are correct. I've been on all three. I'm still here. Barely.
I cried reading this. My mom had a GI bleed last year. She was on sertraline and naproxen for her arthritis. No one told her. She almost died. I printed this out and gave it to my doctor. He actually listened. I'm so glad this exists.
The algorithmic risk stratification is the real innovation here. 86% accuracy via ML on EHR data? That's a paradigm shift from reactive to predictive care. The PPI co-prescription protocol is just the low-hanging fruit. The future is AI-driven pharmacovigilance at the point of prescribing. We're entering the era of precision safety.
I've been on sertraline for 12 years. Took ibuprofen for migraines. Never had an issue. So this whole thing is just fearmongering. People are too scared to take meds anymore. Just live a little. Your gut will be fine. Also, PPIs are bad. I read it on a blog.
This is the kind of post that saves lives. I shared it with my whole family. My dad is 72, on sertraline and naproxen. He’s switching to celecoxib + omeprazole this week. Thank you for making this so clear. We need more of this.
They say 'ask your doctor' but your doctor doesn't know. I asked mine. He said 'eh, it's fine.' So I googled. Found this. Now I'm on acetaminophen. And I'm alive. You're welcome.