Every time a pacemaker is implanted, an insulin pump is activated, or a surgical tool is used in an operating room, there’s a hidden system working behind the scenes to make sure it won’t fail. That system is quality control in manufacturing-a non-negotiable layer of checks, documentation, and standards designed to keep patients safe. It’s not about perfection. It’s about preventing the one in twenty chance that a device could cause serious harm. And in medical manufacturing, that one in twenty isn’t a statistic-it’s a life.
How Quality Control Stops Harm Before It Starts
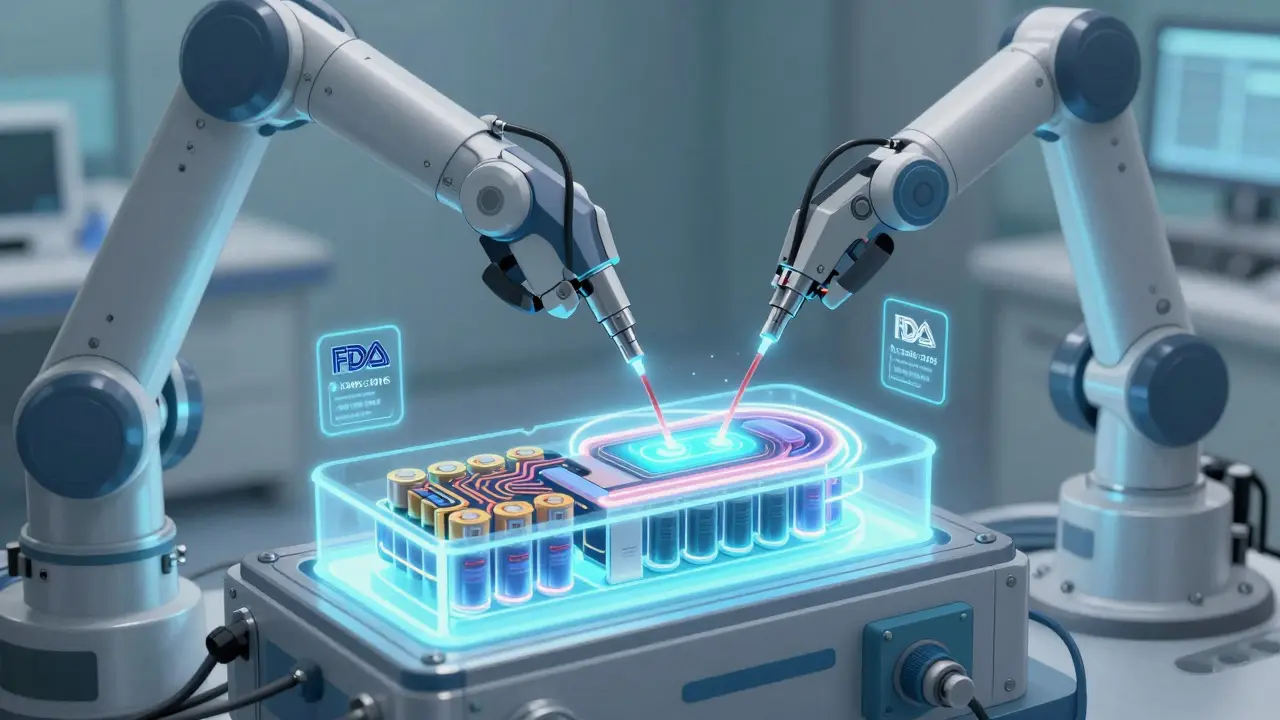
Medical devices aren’t like smartphones or coffee makers. A broken phone is annoying. A faulty ventilator can kill. That’s why quality control in medical manufacturing isn’t optional-it’s enforced by law. The U.S. Food and Drug Administration (FDA) has been shaping these rules since 1978, but the real turning point came in 1996 with the Quality System Regulation (21 CFR Part 820). This regulation laid out 11 core systems manufacturers must follow: from how they design a device to how they handle defective parts. But global supply chains made things messy. A company making heart monitors in Texas might source chips from Germany and assemble them in Mexico. Each country had its own rules. That’s where ISO 13485 came in. Developed by the International Organization for Standardization, this standard became the global language of medical device quality. By 2016, ISO 13485:2016 had become the gold standard, pushing companies to think not just about compliance, but about risk-what could go wrong, how likely it is, and how to stop it before it happens. On January 31, 2024, the FDA made a historic move: it adopted ISO 13485:2016 into its own rules through the Quality Management System Regulation (QMSR). Starting February 2, 2026, U.S. manufacturers will no longer follow two separate rulebooks. They’ll follow one: the same one used by companies in Europe, Canada, Japan, and over 30 other countries. This isn’t bureaucracy-it’s a safety upgrade. It cuts down on redundant paperwork, reduces confusion, and gives manufacturers more time to focus on actual quality, not just filing forms.The Technical Backbone: What Quality Control Actually Looks Like
Quality control isn’t a single step. It’s a chain of checks, each designed to catch errors before they reach a patient. Here’s how it works in practice:- Incoming inspection: Every component-screws, sensors, plastic housings-is tested before it enters production. A single faulty capacitor in a glucose monitor can cause false readings. That’s why incoming parts must meet exact specs, verified with calibrated tools.
- In-process controls: During assembly, statistical process control (SPC) monitors variables like temperature, pressure, and torque. If a machine starts drifting outside acceptable limits, production halts. This isn’t guesswork-it’s math. Domico Med-Device found that using SPC reduced manufacturing errors by up to 45%.
- Final testing: Every finished device undergoes functional testing. Electrical devices must pass IEC 60601-1 standards: a 1,500-volt dielectric test to prevent electric shock, and leakage current limits of 100 microamperes. That’s less than the current needed to feel a tingle on your skin.
- Traceability: Every device has a unique identifier. If a problem arises, manufacturers can pull up its entire history: which batch of material was used, who assembled it, what tests it passed. One company used this to stop a Class I recall before it happened-identifying a software flaw in 5,000 implanted devices just days before shipment.
The Human Factor: Training, Culture, and the Danger of Paper Compliance
You can have the best documentation in the world-and still fail. Dr. Marc Jacobi, a former FDA reviewer, warned that many companies build what he calls “paper quality systems.” They have all the forms, all the signatures, all the procedures… but no real understanding of how things work on the factory floor. That’s why training matters. Production staff need 40 to 80 hours of hands-on training on the specific machines they operate. Quality engineers need 6 to 12 months to master risk analysis under ISO 14971. One quality engineer on Reddit shared that after implementing ISO 13485:2016, their team spent 18 months training everyone across departments. The result? Corrective actions dropped from 45 days to 17. But here’s the catch: 68% of quality managers say they spend too much time on paperwork. The FDA’s own inspection data shows 23% of findings are about “inadequate process validation”-meaning companies followed the checklist but didn’t prove their process actually works. Quality isn’t a folder. It’s a habit. It’s asking, “What if this fails?” before you even start the machine.
Why This Matters Now: The 2026 Deadline and What’s Next
The big shift is coming. February 2, 2026, is the hard deadline. After that, U.S. manufacturers must comply with the new QMSR-ISO 13485:2016 as the law. The FDA gave companies two years to adapt. Most large firms are already halfway there. But smaller companies, especially those with fewer than 50 employees, are struggling. They don’t have teams of compliance officers. They don’t have budgets for expensive software. That’s where tools like Greenlight Guru come in. Used by over 140 medical device companies, this platform offers pre-built templates for FDA and ISO compliance. Users report 32% higher audit success rates. But software alone won’t fix culture. The real advantage comes from integrating quality into daily work-not treating it as a separate department. Looking ahead, two trends are reshaping the future:- AI in quality control: Early adopters are using machine learning to predict defects. By analyzing data from sensors on assembly lines, AI spots patterns humans miss. One study showed a 25-40% drop in defects using this approach.
- Cybersecurity integration: With more devices connected to networks-like smart infusion pumps and remote monitoring implants-ISO is working on updates for 2025 to include cybersecurity risk management. A hacked insulin pump isn’t a data breach. It’s a life-threatening event.
What You Need to Know If You’re in the Industry
If you work in medical manufacturing, here’s what you should do right now:- Know your deadline: February 2, 2026. No extensions. No grace periods.
- Map your gaps: Compare your current system to ISO 13485:2016. Where are you out of sync? Focus on risk management, supplier controls, and design traceability.
- Train your team: Don’t wait. Start with leadership. Then move to production and quality staff. Use free FDA resources like the updated Quality System Manual.
- Fix supplier issues: 41% of FDA warning letters in 2023 cited poor supplier oversight. Audit your vendors. Require proof of their own ISO certification.
- Don’t over-document: Focus on process understanding, not just signatures. If you can’t explain why a step matters, you’re doing it wrong.
What is ISO 13485:2016 and why does it matter for patient safety?
ISO 13485:2016 is the international standard for quality management systems in medical device manufacturing. It requires companies to systematically manage risks, ensure consistent production, and maintain full traceability of every device. Unlike older standards, it embeds risk-based thinking into every process-from design to supplier selection. This means potential failures are identified and stopped before they reach patients. The FDA’s adoption of this standard in 2026 ensures global alignment, reducing confusion and improving safety across borders.
How does the FDA’s new QMSR rule change things for U.S. manufacturers?
Before 2026, U.S. manufacturers had to follow two sets of rules: the FDA’s 21 CFR Part 820 and ISO 13485:2016 for international sales. The new QMSR replaces Part 820 with ISO 13485:2016 as the official U.S. standard. This eliminates redundant paperwork, cuts compliance costs by an estimated $400 million annually, and simplifies global market access. Manufacturers now have one clear path to meet both U.S. and international requirements.
What happens if a medical device manufacturer doesn’t comply by February 2026?
Non-compliance after February 2, 2026, means products can no longer be legally sold in the U.S. The FDA can issue warning letters, seize inventory, or halt production. Companies may also face lawsuits if a non-compliant device causes patient harm. For many, this means losing access to the world’s largest medical device market. The risk isn’t just financial-it’s reputational and ethical.
How do traceability matrices improve patient safety?
Traceability matrices link every design requirement to the final product test results. If a component fails, manufacturers can instantly identify which devices were made with it, where they were shipped, and what risks they pose. This allows for targeted recalls instead of mass withdrawals. One manufacturer used this to prevent a Class I recall by catching a software bug in 5,000 implanted devices before they left the facility-saving lives and millions in costs.
Are there real-world examples of quality control preventing patient harm?
Yes. The FDA estimates quality systems prevent about 200,000 adverse events each year. In one case, a company using ISO 14971 risk management caught a design flaw in a ventilator’s oxygen sensor that could have caused fatal under-dosing. Another found that a batch of syringes had inconsistent needle sharpness-only detectable through statistical process control-before any were distributed. These aren’t hypotheticals. They’re daily realities in well-run facilities.
Can AI really make quality control better?
Absolutely. AI analyzes data from sensors on production lines to detect subtle patterns humans miss-like a slight vibration in a machine that predicts a future failure. Early adopters report 25-40% fewer defects. AI doesn’t replace people-it empowers them. It handles repetitive analysis so quality teams can focus on solving root causes, not just spotting symptoms.


Been in med device QA for 12 years. The shift to ISO 13485:2016 was painful at first, but now? We actually have time to breathe. No more double documenting everything just because the FDA and EU spoke different languages.
Real quality isn’t in the binders. It’s in the guy who stops the line because a screw looks funny.
Let’s be real - most companies treat compliance like a Netflix subscription. They pay the monthly fee, watch the first episode, then forget it exists until the bill comes due. The FDA’s new rule isn’t a burden. It’s a wake-up call for the 68% of quality teams drowning in paperwork while the machines quietly fail.
People don’t get it. Quality control isn’t about rules. It’s about love. Love for the person who’s going to have that pacemaker. Love for their kid who’ll grow up without a funeral. Love for the nurse who has to clean up the mess when something goes wrong.
And if you’re still using clipboards and Excel sheets in 2025? You’re not just behind. You’re dangerous.
❤️
I’ve read through the QMSR draft and ISO 13485:2016 side-by-side. The alignment is actually elegant. The old 21 CFR Part 820 was built for a pre-digital era - think paper logs, handwritten batch records, and inspectors showing up with clipboards. The new framework treats quality as a living system, not a static checklist. What’s missing? More emphasis on human factors in design validation. Engineers still treat operators as error sources, not collaborators. We need more co-design between QA and floor staff - not just training, but shared ownership. The 18-month training rollout mentioned? That’s the gold standard. Not because it’s long, but because it’s deep.
So you’re telling me I gotta pay more so some guy in Germany can sleep better? Why don’t we just make all the devices outta rubber and call it a day?
Let me tell you what happened last quarter at our plant - we caught a batch of insulin pump batteries that were 0.2% out of spec on internal resistance. Not because of a test. Because a technician, who’d been trained on risk mapping under ISO 14971, asked ‘What if this doesn’t fail today… but fails in a patient’s home?’
That’s not compliance. That’s courage.
And yes, we lost $200k in scrap. But we saved a life. And that’s the only ROI that matters.
There’s a quiet metaphysics to quality control. It’s the tension between perfection and pragmatism. We chase zero defects, but we know zero is impossible. So we build systems that assume failure - not to accept it, but to contain it. Every traceability tag, every SPC chart, every risk matrix is a ritual. A prayer, really. A way of saying: ‘I see you, human. I won’t let your body become a statistic.’
It’s not engineering. It’s ethics made visible.
In India, we don’t have the budget for AI-driven QC or Greenlight Guru. But we have something better - elders. The old engineers who’ve seen three generations of devices. They don’t use software. They use their hands, their eyes, their memory. One of them once stopped a line because a wire felt ‘too stiff.’ Turned out the insulation had a micro-crack from a bad batch. No machine detected it. He did.
Technology helps. But wisdom? That’s timeless.
ISO 13485:2016’s risk-based approach is a game-changer, but only if you’re not just doing FMEA as a checkbox. The real win is when your risk register evolves with your process - not the other way around. Also, supplier qualification needs to be dynamic, not annual. One-time audits are a relic. Continuous monitoring via digital twin data? That’s where the future is.
Look, I used to think QA was the department that said ‘no.’ Now I know they’re the ones saying ‘yes’ - yes to safety, yes to trust, yes to life. Every time someone in compliance pushes back on a shortcut, they’re not being annoying. They’re holding the line between a kid and a coffin.
So next time you see a QA person in the hallway, say thanks. Not because it’s polite. Because it’s true.
QMSR adoption requires revalidation of all critical processes under the new ISO framework. That’s not trivial. Especially for legacy devices grandfathered in under Part 820. The FDA’s guidance on transition paths is still ambiguous on design history files. Vendors need clarity on whether legacy DHRs are sufficient or if full re-documentation is mandatory. This is a regulatory minefield.
They spent $400 million on paperwork savings. Meanwhile, patients still die from faulty devices. Who’s really winning here?
Let’s not pretend this is about safety. It’s about control. The FDA doesn’t care about your patients. They care about liability. If a device fails, they want someone to blame. This rule just makes it easier to point fingers. Real safety? That’s when companies stop outsourcing to countries with no oversight. But no one wants to say that out loud.
ai is gonna fix everything. just let the robots do the work. no more humans. no more mistakes. easy.