Obesity and Sleep Apnea: How Weight Affects Breathing at Night
When you carry extra weight, especially around your neck and belly, it doesn’t just change how your clothes fit—it can literally block your airway while you sleep. This is the core link between obesity and sleep apnea, a condition where breathing repeatedly stops and starts during sleep due to blocked airways. It’s not just a theory—it’s why nearly 70% of people with obstructive sleep apnea are overweight or obese. The fat around your neck presses down on your throat, and belly fat pushes up on your diaphragm, making it harder for your lungs to expand. This isn’t about being lazy or out of shape; it’s about physics, biology, and how your body responds to excess weight.
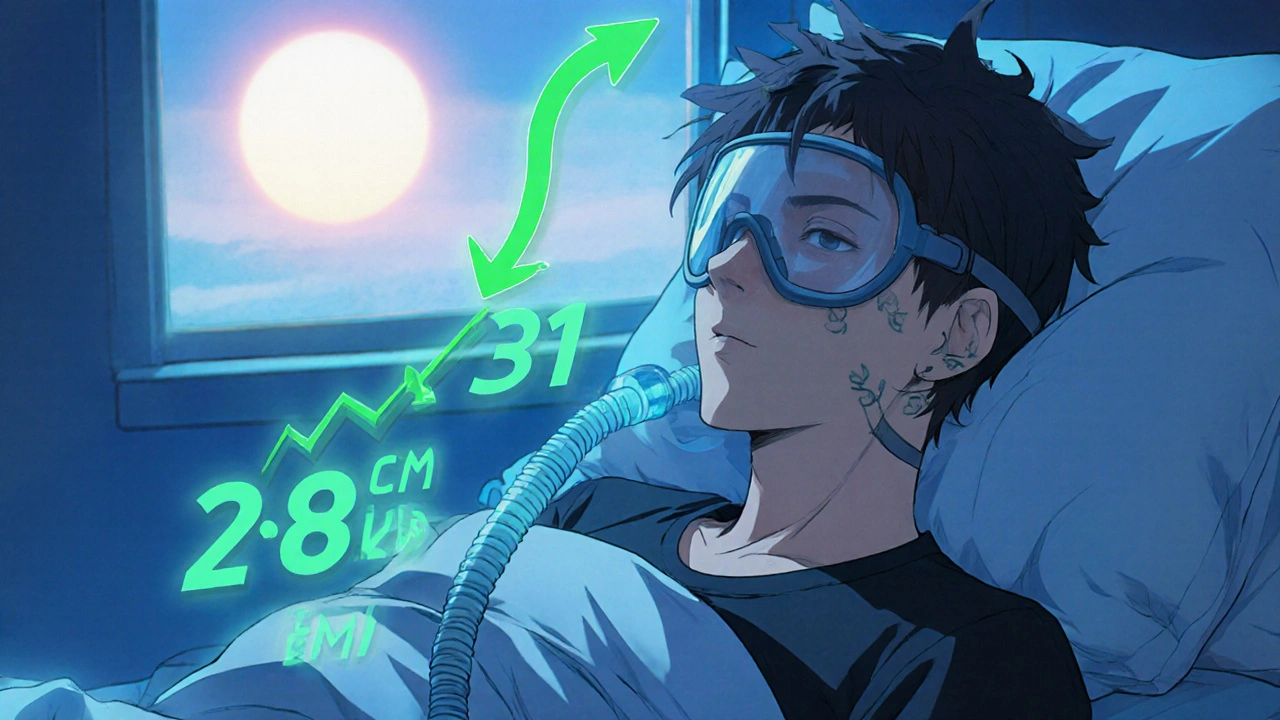
That’s why weight loss and sleep apnea, the connection between shedding pounds and improving nighttime breathing is one of the most proven, life-changing relationships in medicine. Studies show that losing just 10% of your body weight can cut sleep apnea severity by half in many cases. It’s not magic—it’s science. When you lose fat, your airway opens up. Your breathing becomes smoother. Your oxygen levels rise. And suddenly, you’re not waking up gasping, tired, or with a pounding headache every morning. This isn’t just about better sleep—it’s about reducing your risk of heart disease, stroke, and high blood pressure, all of which spike when sleep apnea goes untreated.
And it’s not just about diet and exercise. obstructive sleep apnea, a sleep disorder caused by physical blockage of the airway during sleep often needs more than lifestyle changes. CPAP machines, oral devices, and even surgery can help—but they work best when paired with weight management. Many people feel stuck: they’re too tired to exercise, and their sleep apnea makes it harder to lose weight. That cycle is real. But breaking it starts with understanding the connection. You don’t need to lose 50 pounds overnight. Even small, steady progress can lead to big improvements in how you feel, breathe, and live.
What you’ll find in the posts below isn’t just a list of treatments. It’s a practical guide to what actually works—how medications, lifestyle shifts, and medical tools interact with your body when obesity and sleep apnea are both in play. You’ll see real examples of how people turned things around, what side effects to watch for, and why some common advice misses the mark. This isn’t about quick fixes. It’s about understanding the root cause—and taking steps that stick.
Your BMI directly affects how much pressure your CPAP machine needs to work. Losing even 5-10% of your weight can slash sleep apnea severity and reduce CPAP pressure-sometimes eliminating the need for it entirely.