CPAP Pressure: What It Is, How It Works, and What to Watch For
When you have sleep apnea, your airway collapses when you sleep—cutting off oxygen and waking you up, often without you even realizing it. CPAP pressure, the steady stream of air delivered by a machine to keep your airway open during sleep. Also known as continuous positive airway pressure, it’s the most common and effective treatment for obstructive sleep apnea. Without it, your body struggles to breathe, your heart works harder, and your sleep stays broken. But CPAP pressure isn’t one-size-fits-all. Too low, and your airway still closes. Too high, and you feel like you’re breathing through a straw, your nose gets dry, and you might stop using the machine altogether.
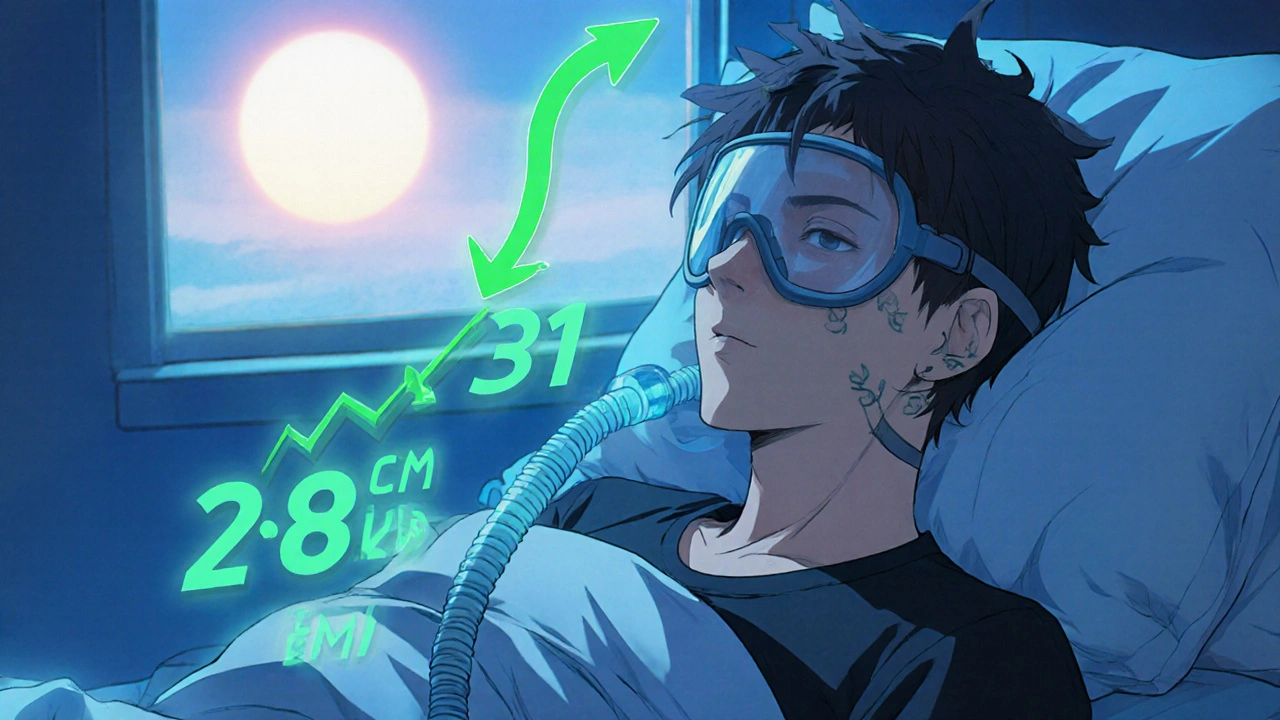
Setting the right CPAP pressure isn’t just about what the machine reads—it’s about what your body actually needs. A sleep study, usually done in a lab or at home, measures how much pressure is needed to stop your breathing pauses. Most people need between 6 and 14 cm H₂O, but some need more, especially if they’re overweight or have severe apnea. The machine doesn’t guess—it adjusts based on your breathing patterns. Some newer models even auto-adjust pressure through the night, responding to snoring, airflow changes, or apnea events. That’s called APAP, or auto-titrating CPAP. It’s not always better than fixed pressure, but for some, it means fewer headaches and more consistent use.
CPAP pressure doesn’t work in isolation. It’s tied to your mask fit, your sleep position, and even your nasal health. A leaky mask? The machine might think you’re having an apnea and ramp up pressure, making it harder to sleep. A stuffy nose? You’ll end up breathing through your mouth, which dries out your throat and makes you quit. That’s why many people start with a humidifier, and why nasal sprays or saline rinses are often part of the routine. It’s also why some switch from a nasal pillow to a full-face mask—if they’re mouth breathers, the pressure won’t stay where it’s supposed to.
And then there’s the human factor. You might feel fine at first, but after a few weeks, you notice you’re tossing and turning more, or you wake up with a dry mouth. That’s not normal. It’s not just "getting used to it." It could mean your pressure needs tweaking. Many people don’t realize they can call their sleep clinic or DME provider for a pressure check. You don’t need another sleep study—you just need someone to review your machine’s data. Most modern CPAP machines store nightly usage, leak rates, and pressure logs. That data tells your doctor if you’re getting enough pressure, or if you’re fighting the machine.
CPAP pressure is the foundation of sleep apnea treatment, but it’s only as good as how well it’s matched to you. It’s not a set-it-and-forget-it device. It’s a tool that needs attention, adjustment, and sometimes a little trial and error. The goal isn’t just to stop snoring—it’s to help you wake up feeling rested, not drained. And that starts with getting the pressure right.
Below, you’ll find real-world guides on how to troubleshoot CPAP issues, what to do when pressure feels off, how to handle side effects, and how to work with your doctor to fine-tune your therapy. These aren’t theory pieces—they’re stories from people who’ve been there and found solutions that actually work.
Your BMI directly affects how much pressure your CPAP machine needs to work. Losing even 5-10% of your weight can slash sleep apnea severity and reduce CPAP pressure-sometimes eliminating the need for it entirely.