BMI: What It Really Means for Your Health and Medication Safety
When you hear BMI, a simple calculation based on height and weight used to estimate body fat. Also known as body mass index, it's one of the first numbers a doctor checks—not because it tells the whole story, but because it quickly flags potential risks like diabetes, heart disease, or drug toxicity. It’s not perfect, but it’s a starting point that connects directly to how your body handles medications.
Think about it: if you have a high BMI, your liver and kidneys might process drugs differently than someone with a lower number. That’s why dosing for painkillers, antidepressants, or even antibiotics often changes based on weight. A drug that works fine at 150 pounds might be too strong—or too weak—at 250. Even something as common as acetaminophen can build up to dangerous levels in people with obesity, because fat tissue changes how the liver breaks it down. And it’s not just about dose. Medications for diabetes, high blood pressure, or cholesterol are chosen partly based on BMI because excess weight affects how well they work. A GLP-1 agonist like semaglutide might be prescribed not just for blood sugar, but because it also helps with weight loss. That’s BMI influencing treatment choices in real time.
On the flip side, low BMI can be just as risky. People with very low body weight often experience stronger side effects from drugs because there’s less tissue to absorb and distribute them. That’s why chemotherapy doses are carefully calculated, and why some antidepressants cause dizziness or fainting in underweight patients. Even something like statins—used to lower cholesterol—can cause muscle damage more easily in people who are underweight. It’s not about being "fat" or "thin." It’s about how your body’s composition affects every pill you take.
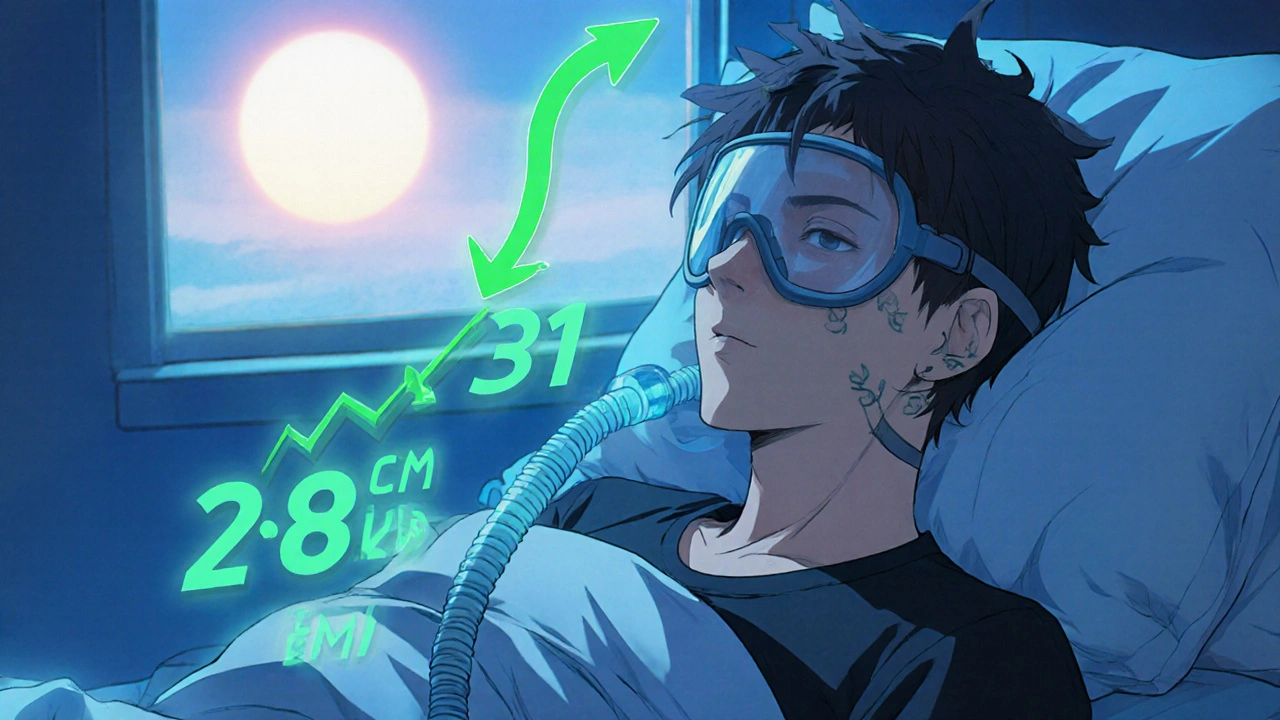
And it’s not just drugs. BMI ties into conditions that show up in half the posts here: sleep apnea, fatty liver disease, joint pain, and even how well glaucoma eye drops work. People with higher BMI are more likely to need medications for multiple issues at once, which increases the chance of dangerous interactions—like mixing opioids with antidepressants or caffeine with ADHD meds. That’s why knowing your BMI helps pharmacists spot risks before they happen.
Below, you’ll find real guides that connect BMI to medication safety, side effects, and treatment choices—not theory, but what actually happens in clinics and pharmacies. Whether you’re managing weight-related diabetes, worried about drug interactions, or just trying to understand why your doctor asked for your height and weight again, these posts give you the facts you need to ask better questions and stay safe.
Your BMI directly affects how much pressure your CPAP machine needs to work. Losing even 5-10% of your weight can slash sleep apnea severity and reduce CPAP pressure-sometimes eliminating the need for it entirely.