When you take a medication like levothyroxine or tacrolimus, you might not think twice about switching from one generic version to another-especially if your pharmacy runs out of the brand you’re used to. But for drugs with a narrow therapeutic index (NTI), that switch can matter more than you realize. These aren’t ordinary pills. A tiny change in how much of the drug gets into your bloodstream can mean the difference between treatment working and something going seriously wrong-like a seizure, organ rejection, or dangerous bleeding.
What Makes a Drug an NTI Drug?
NTI drugs have a razor-thin line between being effective and being toxic. Think of it like walking a tightrope: one small misstep, and you’re falling. The FDA doesn’t publish a full list of these drugs, but it does call out key ones: warfarin, digoxin, lithium, phenytoin, carbamazepine, cyclosporine, and tacrolimus. For these, the margin between a good dose and a dangerous one is often just 2 to 4 times apart. For comparison, most antibiotics have a safety margin of 100 times or more.
That’s why the FDA treats them differently. While regular generics only need to deliver 80% to 125% of the brand-name drug’s effect, NTI generics must hit a tighter window: 95% to 105%. That’s a big deal. It means every batch of a generic NTI drug has to be nearly identical to the original-not just close, but almost the same. Even then, some experts still worry.
Why Switching Between Generics Can Be Risky
Here’s the tricky part: two generics can both be FDA-approved and still behave differently in your body. That’s because they’re made by different manufacturers using different fillers, coatings, or manufacturing processes. The active ingredient might be the same, but how it’s delivered isn’t always identical.
Take tacrolimus, used after organ transplants. A 2019 study looked at four different generic versions and found their active ingredient content ranged from 86% to 120% of the brand. That’s a huge swing-even though all were technically within FDA limits. One patient might get 93% from one pill, then 110% from the next. For someone whose immune system is barely held in check, that spike could mean rejection. A dip could mean infection.
Real-world data backs this up. A 2015 study of kidney transplant patients showed a 21.9% variation in tacrolimus blood levels when patients switched between manufacturers. That’s not random noise-it’s clinically meaningful. Some patients had acute rejection episodes after switching. Others had to be hospitalized for toxicity.
Same story with warfarin. Even though studies show no big spike in bleeding events overall, one 2019 study found switching between generic manufacturers increased INR variability by 0.32 points. For someone on warfarin, that’s like going from a safe zone to the edge of danger. It doesn’t happen to everyone-but when it does, it can be life-threatening.
What Does the Science Actually Say?
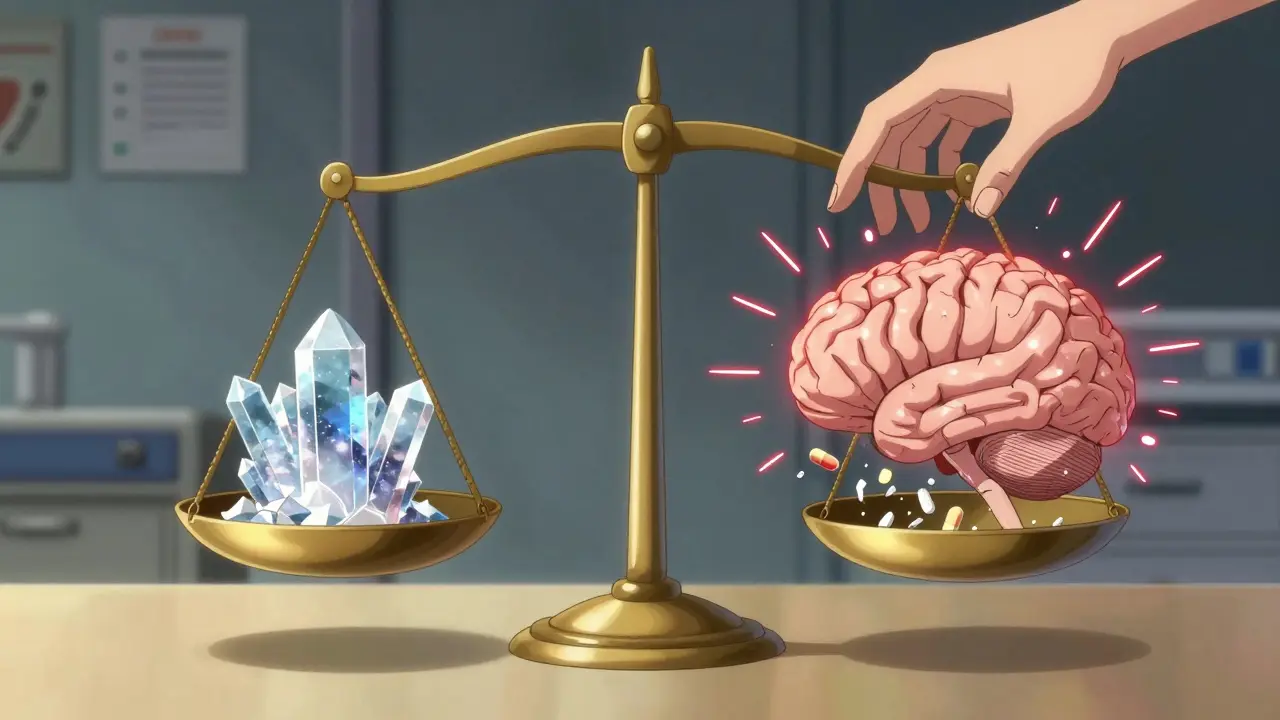
The FDA says generic NTI drugs are therapeutically equivalent. And in large population studies, that’s mostly true. A 2021 FDA review of over 10,000 patients on generic levothyroxine found no meaningful difference in TSH levels compared to brand-name Synthroid. The average difference? 0.03 mIU/L-statistically invisible.
But science doesn’t always tell the whole story. Population averages don’t capture individual sensitivity. One person might handle a switch fine. Another, with a slower metabolism or a sensitive thyroid, might crash into hypothyroidism. That’s why doctors and pharmacists still hesitate.
A 2019 national survey of pharmacists found that while 87% believed generics were just as effective, 63% had received complaints from patients or doctors after switching NTI generics. These weren’t just anecdotes-they were reports of fatigue, weight gain, seizures, or elevated liver enzymes. And in states with laws restricting NTI substitution, pharmacists are far less likely to switch without explicit permission from the prescriber.
What’s the Real-World Impact?
Let’s say you’re on carbamazepine for epilepsy. You’ve been stable for two years. Then your insurance changes, and your pharmacy switches you to a different generic. Within weeks, you have a seizure. You go back to the original brand, and you’re fine again. This isn’t rare. The Epilepsy Foundation collects hundreds of these stories.
Even the American Academy of Neurology says: don’t automatically substitute antiepileptic NTI drugs. Why? Because in some patients, even a 5% change in blood concentration can tip the balance. And we still don’t have good tools to predict who’s vulnerable.
Same with lithium. A 0.2 mmol/L shift in blood level can turn a calm mood into mania-or worse, toxicity. One study found that patients who switched manufacturers were twice as likely to be hospitalized for lithium-related issues.
These aren’t edge cases. They’re real people. And they’re not outliers-they’re the ones who slip through the cracks of population-level data.
What Should You Do?
If you take an NTI drug, here’s what you need to know:
- Ask your doctor if your drug is on the NTI list. If it is, ask whether switching is safe for you.
- Check your prescription. Some states require the prescriber to write “Do Not Substitute” on NTI prescriptions. If you don’t see that, ask why.
- Track your symptoms. If you feel different after a switch-more tired, more anxious, having more seizures, or noticing unusual bruising-tell your doctor immediately.
- Request consistent manufacturers. If your pharmacy switches brands, ask if they can stick with the same one. Many pharmacies will honor that if you ask.
- Get blood tests. For drugs like warfarin, lithium, or tacrolimus, regular monitoring isn’t optional-it’s essential. Don’t skip them.
There’s no perfect answer. The FDA’s data says generics are safe. But real-world experience says: proceed with caution. For some people, switching between NTI generics is harmless. For others, it’s a gamble they can’t afford to take.
What’s Being Done?
The FDA is tightening its rules. Since 2018, they’ve required more in vivo testing for drugs like tacrolimus and cyclosporine-not just lab tests, but actual human studies. That’s because in vitro data doesn’t always predict how the body reacts.
Twenty-seven states now have laws that limit or prohibit automatic substitution of NTI drugs. In Minnesota, for example, pharmacists must get explicit permission from the prescriber before switching a patient from one NTI generic to another. Other states require the pharmacist to notify the patient and document the change.
But enforcement is patchy. And patients often don’t know they’ve been switched. That’s why awareness matters.
The Bottom Line
Generic drugs save billions. That’s good. But NTI drugs aren’t like antibiotics or cholesterol pills. They’re precision tools. And like any precision tool, they need consistent use to work right.
The science says most people won’t notice a difference. But the experience of thousands shows that some will. And for those people, the difference isn’t just inconvenient-it’s dangerous.
If you’re on an NTI drug, don’t assume switching is harmless. Ask questions. Monitor your body. Push for consistency. Your health might depend on it.




I took my generic levothyroxine for 3 years, then switched brands and suddenly felt like my body was full of wet cement. No energy. No joy. Just… heavy. I thought it was depression. Turns out? My TSH shot up. I went back to my original brand and boom - I’m human again. Why do they treat our bodies like interchangeable widgets? 🤔
so like… i get that this is a big deal for some ppl, but honestly? my doc just says 'take what they give you' and i've never had an issue. maybe i'm just lucky? 🤷♂️
The FDA’s 95-105% window is a joke. It's not precision. It's a loophole dressed up as regulation. Two batches can differ by 20% in bioavailability and still be 'equivalent.' That's not science. That's corporate convenience masked as public policy. We're not testing drugs. We're testing human endurance.
This is why India produces 40% of the world’s generic drugs and we’re STILL not trusted. You think your 'FDA-approved' generic is safe? Ha. The raw APIs come from our labs - same molecules, different fillers, different binders, different manufacturing chaos. You think your body doesn’t notice? You’re the one who gets sick while the CEO buys a yacht. We don’t need more studies. We need accountability. And someone to hold the hands of the people who actually make the pills while the suits sip champagne.
Let’s be real. The entire generic drug industry is a Ponzi scheme built on the backs of people who can’t afford brand names. The FDA doesn’t care about individual variation because they don’t have to. They care about population averages. That’s not medicine. That’s actuarial science disguised as healthcare. And the people who suffer? They’re just noise in the spreadsheet.
If you're on an NTI drug, please talk to your pharmacist. Ask for consistency. Ask for documentation. You have a right to know what you're taking. And if your provider hesitates? Push harder. Your health isn't a cost-cutting metric. It's your life.
Oh honey, you think this is bad? Wait till you find out your 'generic' warfarin was made in a warehouse with a leaking roof and a dog named Barry as quality control. 🙃
The fact that people still believe in 'therapeutic equivalence' for NTI drugs proves how badly we’ve been conditioned to accept corporate lies as medical truth. You don’t need a study. You need a brain. And apparently, most people traded theirs in for a coupon.
I’m so glad someone finally put this out there. My mom had a seizure after switching generics. She’s fine now, but we’ve been screaming at pharmacies ever since. Please, if you’re reading this - don’t let them switch you without asking. You’re not just a prescription number. You’re someone’s daughter. Someone’s mom. Someone’s everything.
This is why Western countries are weak. They let big pharma control everything. In India, we know generics are life - but we also know when to stop. We don’t let some American insurance company decide if your epilepsy drug is 'close enough.' We respect the medicine. You should too.
I work in a pharmacy. I’ve seen patients cry because they switched and got sick. I’ve had doctors scream at me for not asking. But the system doesn’t let us pause. We’re told to swap. We’re told to save money. We’re told not to think. So we don’t. And people suffer because we were trained to be quiet.
There is a profound disconnect between regulatory frameworks and clinical reality. While population-level data may suggest equivalence, individual pharmacokinetic variability - influenced by genetics, gut microbiota, and metabolic pathways - renders this assumption dangerously incomplete. The current paradigm prioritizes scalability over safety. This is not sustainable.
i think this is super important but i also think we need to make it easier for people to know if they've been switched. like, maybe the pill should have the manufacturer name printed on it? or a little sticker? i had no idea mine changed until i got sick. i'm so tired of being treated like a lab rat. <3