
EPO-Antipsychotic Interaction Risk Checker
Your Risk Assessment
Enter your medication details to understand your potential seizure risk when taking evening primrose oil.
How This Works
Based on medical research and the article content, this tool assesses your seizure risk when taking evening primrose oil with antipsychotics. Your risk is determined by your specific medication and seizure history.
Recommendations
It’s 2025, and you’re taking an antipsychotic like quetiapine or risperidone. You’ve heard evening primrose oil helps with PMS, eczema, or joint pain. So you grab a bottle. But your pharmacist pauses. "Wait-do you have epilepsy? Or a history of seizures?" That question stops you. Because here’s the problem: evening primrose oil might lower your seizure threshold. Or maybe it doesn’t. The truth is messy, conflicting, and deeply personal.
What Even Is Evening Primrose Oil?
Evening primrose oil comes from the seeds of a yellow-flowered plant called Oenothera biennis. It’s been sold for decades as a natural remedy. Its main active ingredients are linoleic acid and gamma-linolenic acid (GLA). GLA turns into prostaglandin E1 in your body-a compound with real anti-inflammatory power. That’s why people take it for breast pain, dry skin, or arthritis. But that same chemistry is what makes neurologists nervous.The Seizure Controversy: Two Sides of the Same Coin
In the early 1980s, a few case reports popped up. Someone on EPO had a seizure. Then another. Then another. The story spread. By the 1990s, most pharmacies and health sites added warnings: "Avoid if you have epilepsy." But here’s the twist. In 2007, Dr. BK Puri from Imperial College London dug into every single study ever done on this. His review found no solid proof that evening primrose oil causes seizures. In fact, he found the opposite. In animal models, the fatty acids in EPO actually blocked sodium channels-something many anti-seizure drugs do. Prostaglandin E1, derived from GLA, showed anticonvulsant effects in lab tests. Puri called the seizure link "spurious." He argued that the warnings should be removed. So why do Mayo Clinic, Walgreens, and Familiprix still warn against it? Because in the real world, people still report problems. One case from 2023 described a patient under anesthesia who had a seizure after taking EPO. Another Reddit user with schizophrenia said their neurologist told them to stop it cold. A 2023 survey of 4,500 epilepsy patients found EPO was the #7 most-used supplement in that group. And among those users, 32% said their seizures got worse. That’s not a small number.Antipsychotics: The Hidden Danger Zone
You might think, "I don’t have epilepsy. I’m fine." But if you’re on an antipsychotic, you’re not off the hook. Many of these drugs-like clozapine, olanzapine, and even newer ones like brexpiprazole and lumateperone-can lower the seizure threshold on their own. Add EPO into the mix, and you’re stacking two potential triggers. DrugBank’s latest update (April 2025) lists five antipsychotics with confirmed interaction risks: flupentixol (Fluanxol), chlorpromazine (Largactil), amifampridine, brexpiprazole, and pimavanserin. These aren’t just theoretical. Pharmacists at Walgreens reported a 27% spike in questions about EPO and antipsychotics in 2023 compared to 2022. The Epilepsy Foundation says the risk is "theoretical"-but they still advise caution. The American Academy of Neurology gives EPO the lowest evidence rating (Class IV) for seizure risk. That means no large, solid trials prove it causes seizures. But there’s enough biological plausibility to make doctors nervous.
What the Research Really Says
Let’s cut through the noise. - Animal studies: EPO components reduced seizures in four different epilepsy models. Protective effect. (Puri, 2007) - Human case reports: Dozens of isolated incidents where seizures followed EPO use-often with other drugs involved. - Large population surveys: 32% of epilepsy patients on EPO reported more seizures. 57% said no change. - Pharmacokinetics: GLA peaks in blood 2.7-4.4 hours after ingestion. That’s when your brain is most exposed. - Meta-analysis: No consistent signal of increased seizure risk across controlled trials. But no trials were designed to test this directly. So what’s the answer? There isn’t one. Not yet.The 2024 Study That Might Change Everything
A major clinical trial is underway. Launched in January 2024 by Imperial College London and Johns Hopkins, it’s tracking 300 people with epilepsy who are taking EPO daily. The goal? To see if it truly affects seizure frequency over 18 months. Results won’t be out until late 2025. Until then, you’re left with a choice: trust the animal data and the 2007 review? Or follow the institutional warnings from Mayo Clinic and the Epilepsy Foundation?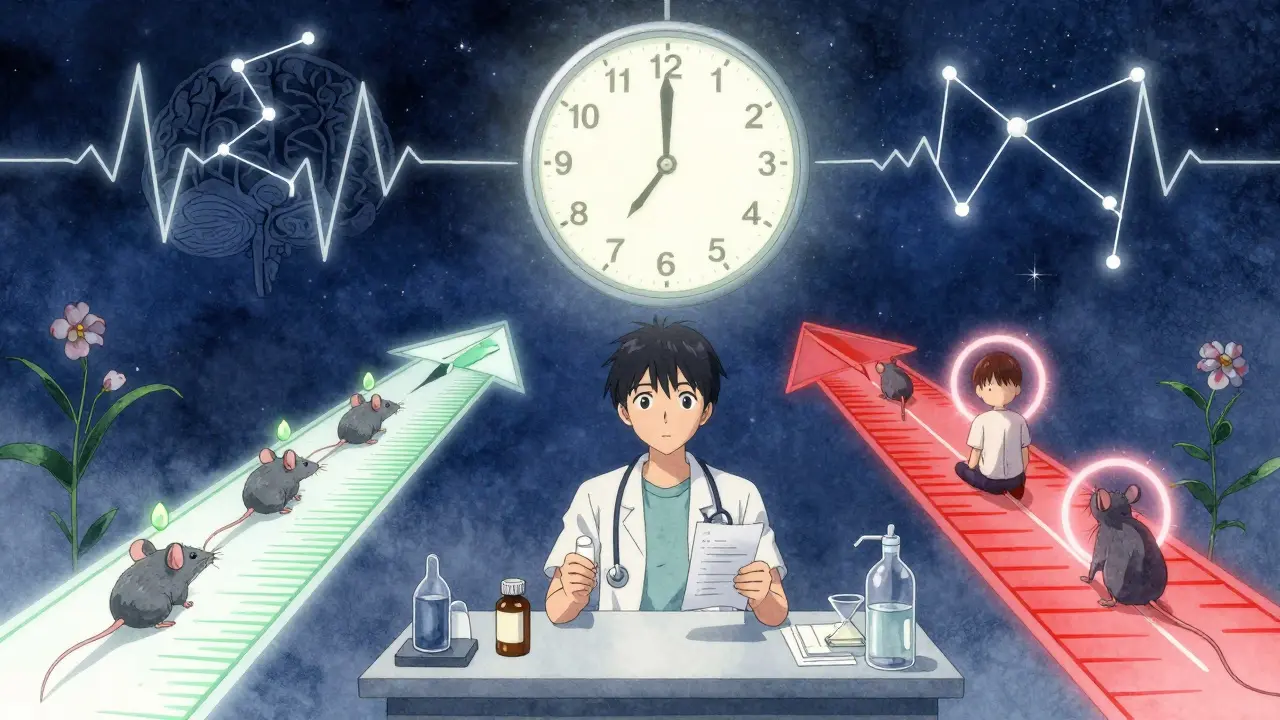
What Should You Do?
If you’re on an antipsychotic or have epilepsy, here’s what to do:- Don’t start EPO without talking to your doctor. Especially if you’re on clozapine, quetiapine, or any drug with a seizure warning.
- Don’t assume it’s safe just because it’s "natural". Supplements aren’t regulated like drugs. Doses vary. One bottle has 500mg GLA. Another has 1,300mg. That’s a huge difference.
- Track your seizures. If you’re already taking EPO and notice more auras, muscle twitches, or confusion-stop and call your neurologist.
- Check your labels. As of Q1 2024, 68% of EPO products include epilepsy warnings. But some don’t. That’s dangerous.
- Consider alternatives. For PMS or skin issues, fish oil (omega-3s) or vitamin B6 have better safety profiles with antipsychotics.
The Bottom Line
Evening primrose oil isn’t a villain. It’s not a miracle cure either. It’s a supplement with real biological activity-and a dangerous gray zone when mixed with psychiatric meds. The science is split. The warnings are inconsistent. The market keeps growing, even as patients report mixed outcomes. Your brain isn’t a lab rat. Your seizures aren’t a theory. If you’re on antipsychotics, your safest move isn’t guessing. It’s asking. Getting your neurologist on the line. Sharing your supplement list. Waiting for the 2025 trial results. Because when it comes to your seizure threshold, there’s no room for doubt.Can evening primrose oil cause seizures in people taking antipsychotics?
Yes, it’s possible. While research is conflicting, multiple case reports and pharmacological data suggest EPO may lower the seizure threshold, especially when combined with antipsychotics like clozapine, quetiapine, or chlorpromazine. DrugBank and Familiprix list specific interactions. Even if the risk is low, it’s not zero-especially if you already have a history of seizures or are on multiple seizure-lowering drugs.
Is evening primrose oil safe if I don’t have epilepsy?
If you’re not on antipsychotics or other seizure-lowering medications, and have no personal or family history of seizures, the risk is likely very low. But that doesn’t mean it’s zero. The 2007 study suggests EPO may even be protective. Still, if you’re unsure, talk to your doctor before starting. There are safer alternatives for skin or hormonal issues.
Which antipsychotics interact most with evening primrose oil?
The strongest documented interactions are with flupentixol (Fluanxol), chlorpromazine (Largactil), amifampridine, brexpiprazole, and pimavanserin. These drugs already carry seizure risk on their own. Adding EPO may push that risk higher. If you’re on any of these, avoid EPO unless your doctor approves it with close monitoring.
Why do some sources say EPO is safe and others say it’s dangerous?
It’s a clash of evidence types. Animal and lab studies show EPO may reduce seizures. But human case reports show seizures happening after EPO use-often alongside other meds. Institutions like Mayo Clinic err on the side of caution because one bad outcome can be devastating. Researchers like Puri argue the evidence is weak and outdated. Until large human trials are complete, both sides will keep arguing.
Should I stop taking evening primrose oil if I’m on an antipsychotic?
If you’re on an antipsychotic and have any history of seizures, neurological disorders, or are taking other medications that lower seizure threshold, stop taking EPO immediately and consult your doctor. Don’t quit your antipsychotic-but do pause the supplement. Your neurologist can help you weigh the benefits of EPO (like reduced PMS pain) against the potential risk of seizures. There are other options.
Are there supplements that are safer than evening primrose oil for PMS or eczema?
Yes. For PMS, vitamin B6, magnesium, and calcium have strong evidence and no known seizure risks. For eczema, fish oil (omega-3s) and topical ceramides are safer and better studied. Avoid borage oil and starflower oil-they’re similar to EPO and carry the same risks. Stick to supplements with proven safety profiles when you’re on psychiatric meds.



OMG I took this for my eczema and had a weird aura last week 😱 I thought it was stress but then I remembered I started EPO right before... my neurologist flipped out. Like, WHY does no one warn you? I’m 28, no history of seizures, but now I’m terrified to even look at a supplement bottle. 🥲
While I appreciate the nuanced exploration of the pharmacological dynamics surrounding evening primrose oil and its potential interaction with antipsychotic agents, I must respectfully submit that the prevailing institutional caution-though seemingly overzealous-is not without merit, particularly when one considers the variable bioavailability of unregulated botanical extracts and the profound neurochemical vulnerability inherent in patients on CNS depressants. One anecdotal case does not a meta-analysis make, but neither does a single 2007 review invalidate decades of clinical prudence. Safety first, always.
bro i was on this for my cramps and my mom freaked out when she saw it in my drawer. she said ‘you’re on risperidone?? why you doing that??’ i didn’t even know it was a thing. now i’m scared to take anything. but i miss my skin being less dry 😭
I get why people are scared. I’ve seen friends go from ‘this oil fixed my PMS’ to ‘I had a seizure and now I’m on three meds.’ But I also know people who’ve taken it for 10 years with zero issues. The problem isn’t the oil-it’s the lack of clear guidance. Why don’t pharmacies print warnings on the bottle? Why do some brands say ‘safe’ and others say ‘dangerous’? We need standardization, not fear-mongering. And yes, fish oil is better-but EPO works. Let’s not throw the baby out with the bathwater.
It’s funny how we treat supplements like they’re either magic or poison. EPO is neither. It’s a molecule with effects. Some people’s brains react to it. Others don’t. The same way some people get seizures from sleep deprivation or caffeine. The real issue isn’t EPO-it’s that we’ve outsourced our medical literacy to pharmacists and Google. We need better education, not blanket warnings. Also, the 2025 trial is going to be wild. I’m putting money on ‘no significant effect.’
Hey everyone-just wanted to say if you’re reading this and feeling anxious, you’re not alone. I’ve been on quetiapine for 5 years and took EPO for 2 years before I found this thread. I stopped it. Switched to magnesium. My skin’s okay, my cramps are manageable, and I sleep better knowing I didn’t risk my brain. You don’t have to be perfect. Just be safe. And if you’re scared to talk to your doctor? Bring this post. I did. They were impressed. You got this 💪
How is this even a debate? The fact that you’re asking whether a plant extract with unregulated dosing and zero FDA oversight is ‘safe’ with CNS drugs suggests you’ve never read a single pharmacology textbook. The 2007 review? A single researcher’s opinion. The Epilepsy Foundation? The gold standard. The 32% of patients who reported worsening seizures? That’s not ‘mixed outcomes’-that’s a red flag waving in a hurricane. If you’re taking antipsychotics and think ‘natural’ means ‘safe,’ you’re one bad batch away from the ER. Stop romanticizing supplements. Your brain isn’t a TikTok trend.
Everyone’s acting like EPO is the devil. What about St. John’s Wort? Or ginkgo? Or kava? Those are way worse. Why is this the only supplement getting demonized? Oh right-because it’s used by women for PMS. Classic. If this was a pharmaceutical drug made by Pfizer, no one would care. But since it’s a ‘hippie oil,’ suddenly it’s a neurotoxin? Wake up. The real danger is fear-based medicine.