Verapamil – What It Is and Why It Matters
If you’ve been told to take verapamil, you probably wonder what the pill actually does. In short, verapamil is a calcium‑channel blocker that helps relax blood vessels and slow down the heart. Doctors use it for high blood pressure, certain rhythm problems, and chest pain caused by reduced blood flow.
Understanding how it works makes it easier to follow your doctor’s advice and spot any issues early. Below we’ll break down the basics, show you how to get the right dose, and point out what to watch for while taking the drug.
How Verapamil Works
Verapamil blocks calcium from entering heart muscle cells and the smooth muscles that line blood vessels. Less calcium means those muscles don’t contract as hard. The result is lower blood pressure and a slower, more regular heartbeat. This effect helps prevent episodes of angina (chest pain) and controls abnormal rhythms like atrial flutter.
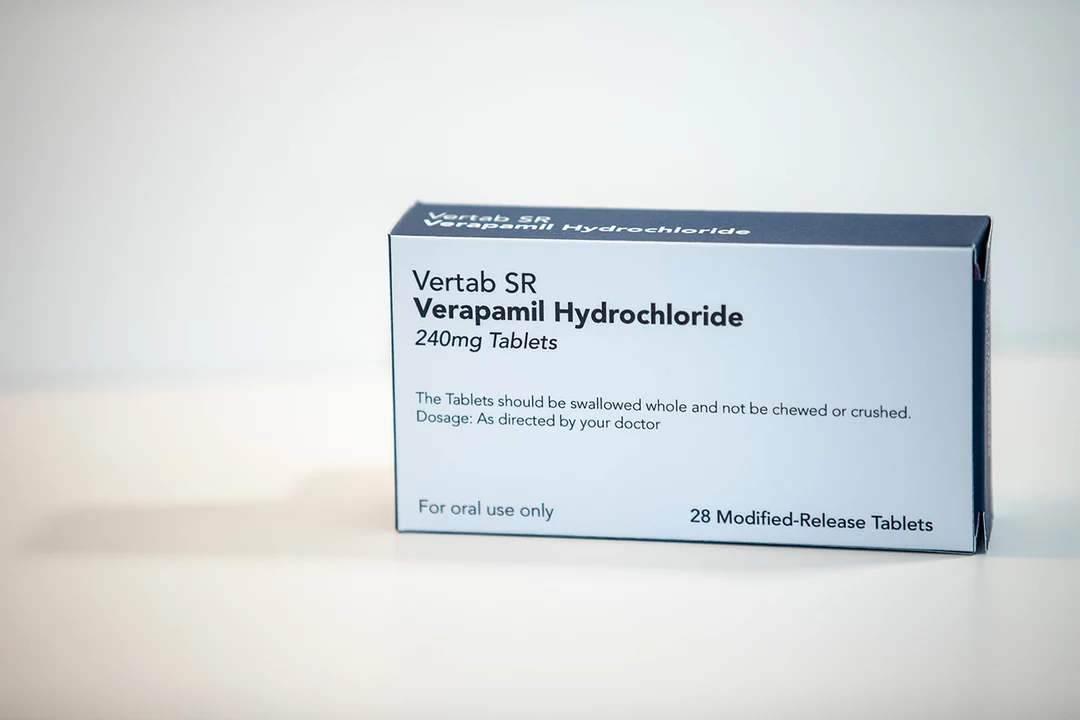
The medication comes in several forms: immediate‑release tablets, extended‑release tablets, and injectable versions for hospital use. Your doctor will pick the form that fits your condition and lifestyle best.
Getting the Right Dose
Dosage varies a lot. For high blood pressure, doctors often start with 80 mg taken three times daily in the immediate‑release version. If you’re on the extended‑release tablet, a typical starting dose is 120 mg once a day, sometimes increased to 240 mg.
When it’s used for rhythm problems, the dose may be lower but taken more frequently—often 40 mg three times a day. Always follow the exact schedule your doctor gives you; missing doses or taking extra pills can cause heart rate changes that feel scary.
If you forget a dose, take it as soon as you remember unless it’s almost time for your next one. In that case, skip the missed pill and continue with your regular schedule. Never double up.
Common Side Effects to Expect
Most people feel fine, but some notice a few side effects. The most common are mild dizziness, headache, or a feeling of tiredness. These usually fade after the body gets used to the medicine.
A slower heart rate (bradycardia) can happen, especially if you’re also on other heart‑affecting drugs. If your pulse drops below 60 beats per minute or you feel faint, call your doctor.
Another possible issue is swelling in the ankles or feet. This happens because blood vessels relax and fluid can collect in lower limbs. Raising your legs and wearing loose socks may help, but tell your doctor if it gets worse.
Safety Tips and Interactions
Verapamil interacts with several other medicines, including some antibiotics, antifungals, and drugs for high cholesterol. Always give your pharmacist a full list of what you’re taking.
Avoid grapefruit juice while on verapamil; it can raise drug levels in the blood and increase side‑effects. Also, if you have severe liver disease or heart failure, let your doctor know—dosage may need adjustment.
Pregnant or breastfeeding women should discuss risks with their healthcare provider, as safety data is limited.
Monitoring and When to Seek Help
Your doctor will likely check blood pressure, heart rate, and sometimes an ECG after you start the medication. Keep a simple log of any new symptoms so you can share it at your next visit.
If you notice chest pain that doesn’t go away, sudden shortness of breath, or severe dizziness, treat it as an emergency and get help right away.
Overall, verapamil is a proven tool for managing blood pressure and certain heart rhythm issues. By taking it exactly as prescribed, watching for side effects, and staying in touch with your doctor, you can keep your heart working smoothly.
As a blogger, I feel it's important to discuss the risks associated with combining Verapamil and alcohol. Verapamil is a medication used to treat conditions like high blood pressure and chest pain, while alcohol is a widely consumed recreational beverage. Combining these two substances can lead to dangerous side effects such as dizziness, drowsiness, and an increased risk of accidents. Additionally, alcohol may reduce the effectiveness of Verapamil, making it harder to control your symptoms. It's crucial for individuals taking Verapamil to understand these risks and avoid consuming alcohol to ensure their safety and the effectiveness of their medication.