Bariatric Medication Adjustment Calculator
After bariatric surgery, many medications require dose adjustments. This tool helps you determine if your medications need adjustment based on your surgery type and the specific drugs you're taking.
Medication Adjustment Recommendations
Key Considerations
Remember: These are general guidelines. Always consult your physician or pharmacist for personalized advice.
After bariatric surgery, many patients are surprised when their medications stop working the way they used to. A pill that once kept blood pressure in check might suddenly seem ineffective. Thyroid medication might need double the dose. Painkillers could stop working entirely. This isn’t imagination-it’s physiology. Bariatric surgery changes how your body absorbs drugs, and if you don’t adjust, you risk serious health consequences.
Why Your Pills Don’t Work Like They Used To
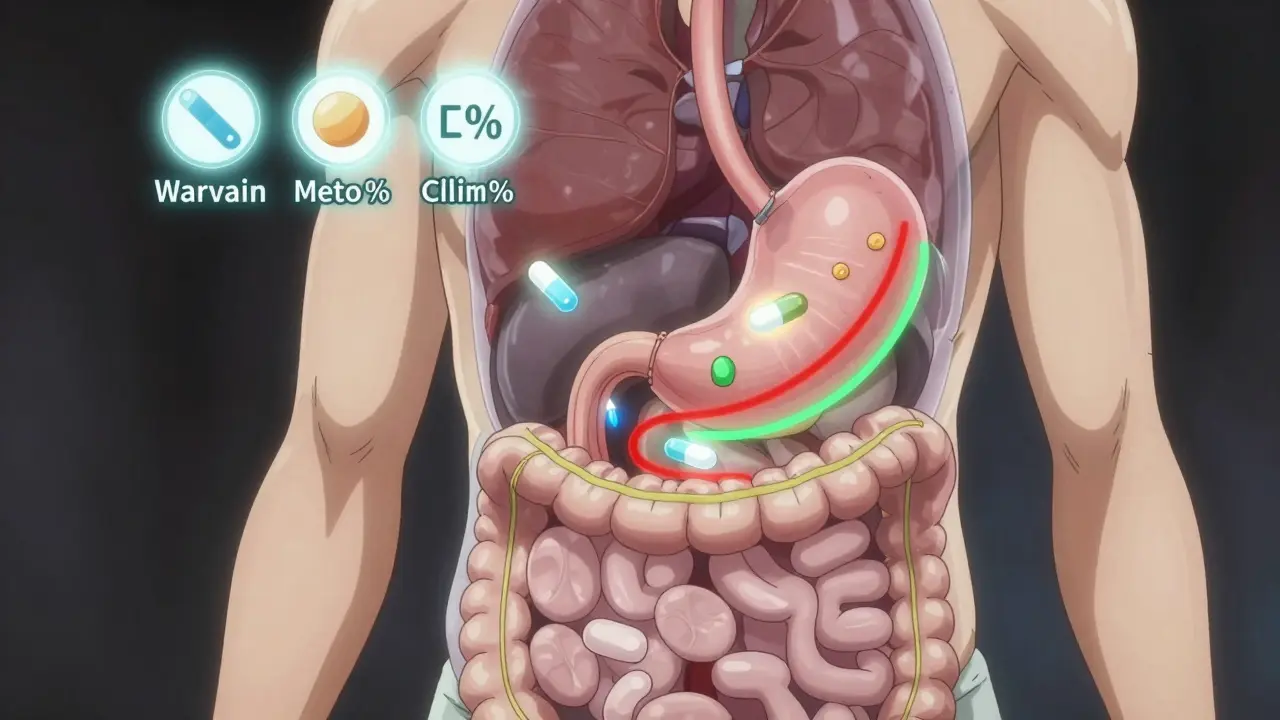
Bariatric surgery isn’t just about shrinking your stomach. It rewires your digestive system. Procedures like Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy alter the path food-and medications-take through your body. Before surgery, a pill would sit in your stomach, dissolve in acid, then move slowly into the small intestine where most drugs are absorbed. After surgery? That path is gone. In RYGB, up to 150 cm of the small intestine is bypassed. That’s about a third of your total absorptive surface. The stomach is reduced to a small pouch, and the pH rises from a strong acid (1.5-3.5) to a much weaker one (4.0-6.0). That’s a problem for drugs that need acid to dissolve, like itraconazole or ketoconazole. Extended-release pills? They’re designed to release slowly over hours. But with food moving through your system 40% faster, those pills can zip right through without releasing their full dose. Studies show 40-60% of extended-release formulations lose effectiveness after RYGB. Even sleeve gastrectomy, which doesn’t bypass the intestine, still changes things. The stomach is now 100-150 mL instead of 1,000-1,500 mL. That means tablets don’t have room to dissolve properly. Many patients report pills “not dissolving” or feeling like they’re stuck. And with less acid, drugs that need an acidic environment to be absorbed become less effective.Which Medications Are Most Affected?
Not all drugs are impacted the same. Some are more sensitive to changes in pH, transit time, or surface area. Here are the big ones:- Levothyroxine (thyroid hormone): Bioavailability drops 25-30% after RYGB. Many patients need a 20-50% dose increase. One study found a patient’s dose had to jump from 75 mcg to 125 mcg after surgery.
- Metformin ER: Plasma concentrations drop 30-40%. The extended-release version often fails completely. Doctors now recommend switching to immediate-release metformin, taken 2-3 times daily.
- Glipizide XL: This diabetes pill lost 50-75% of its effectiveness after bypass. Patients saw spikes in blood sugar despite taking the same dose.
- Oxycodone CR: Bioavailability fell by 60%. Patients reported pain returning sooner and more intensely.
- Warfarin: A blood thinner with a narrow safety window. In 60% of RYGB patients, doses had to be increased by 25-35% to maintain therapeutic levels. Too little? Risk of clots. Too much? Risk of bleeding.
- Calcium and Vitamin D: Absorption drops 35% after bypass. Nearly 72% of patients need higher doses post-surgery to prevent bone loss.
- Enteric-coated pills: These are designed to dissolve in the small intestine, not the stomach. But with faster transit and altered pH, they often dissolve too early or too late, leading to inconsistent absorption.

Procedure Matters: Not All Surgeries Are the Same
The type of surgery you had makes a huge difference in how your meds behave.- Roux-en-Y Gastric Bypass (RYGB): Causes the most dramatic changes. Bypasses the duodenum-the part of the intestine where many drugs are absorbed. About 68% of RYGB patients need medication adjustments.
- Sleeve Gastrectomy: Mostly restricts food intake. Only 15-20% of drug bioavailability is lost. But gastric pH still rises, so acid-dependent drugs still suffer. Only 32% of sleeve patients need changes.
- Biliopancreatic Diversion (BPD/DS): The most extreme malabsorptive surgery. Drops drug absorption by 50-70%. Rare (only 2.5% of cases) but requires the most aggressive dosing changes.
- Adjustable Gastric Band: Minimal impact on anatomy. But because food intake drops 70-80%, drugs that need food to absorb (like mycophenolate) become less effective. Dose increases of 30-40% may be needed.
What Should You Do? Practical Steps
You can’t just keep taking the same pills the same way. Here’s what works:- Switch extended-release to immediate-release. This is the #1 recommendation from the American Society for Metabolic and Bariatric Surgery. For example, switch metformin ER to regular metformin taken twice daily. Same with glipizide XL-use glipizide twice a day.
- Use liquids or crush pills (if safe). In the first 3 months after surgery, liquid formulations are preferred. For pills that can be crushed (check with your pharmacist), this helps with dissolution. Never crush enteric-coated or extended-release pills unless instructed.
- Time your doses carefully. Take acid-dependent drugs (like levothyroxine) on an empty stomach, 30-60 minutes before meals. Take fat-soluble drugs (like some antifungals) with meals. Some drugs work better with food, others worse.
- Get therapeutic drug monitoring. For drugs like warfarin, phenytoin, cyclosporine, and lithium, regular blood tests are essential. Target levels post-surgery are different than before. Your doctor should check levels within 4-6 weeks after surgery, then every 3-6 months.
- Track your symptoms. If your pain returns, your thyroid feels off, or your blood sugar spikes, it might not be your condition worsening-it might be your pill not working.
What You Need to Tell Your Doctor and Pharmacist
Most providers aren’t trained in this. A 2022 survey found 78% of community pharmacists had little to no training in post-bariatric medication management. Don’t assume they know. Be specific:- “I had a Roux-en-Y gastric bypass in 2023.”
- “I used to take metformin ER 1000 mg once daily. Now I feel dizzy and my sugar is high. What should I do?”
- “I’m taking levothyroxine but my TSH went up. Is it the surgery?”
The Bigger Picture: Why This Is Getting More Attention
Bariatric surgery is booming. Over 721,000 procedures were done worldwide in 2022. As more people have surgery, more are running into these drug issues. The FDA added bariatric-specific warnings to 17 drug labels between 2022 and 2023. The European Medicines Agency now requires all new oral drugs to include bariatric absorption data. In the U.S., 42 pharmacy schools now teach bariatric pharmacotherapy-up from 12 in 2019. New tools are emerging. AI-powered dosing calculators are now used in 83 U.S. hospitals. pH-adaptive capsules are in clinical trials, designed to dissolve even in weak stomach acid. Subcutaneous implants like ITCA 650 (for diabetes) are proving more reliable than pills after surgery. But the most powerful tool you have? Awareness. If you had bariatric surgery and your meds aren’t working, it’s not your fault. It’s a known, documented, and solvable problem. Don’t wait for symptoms to get worse. Talk to your doctor. Ask your pharmacist. Get your levels checked. Adjust your doses. Your health depends on it.Do all bariatric surgeries affect medication absorption the same way?
No. Surgeries that bypass parts of the small intestine-like Roux-en-Y gastric bypass and biliopancreatic diversion-cause the most significant changes. Sleeve gastrectomy, which only reduces stomach size, has a milder effect. Gastric banding has the least impact, mainly affecting food-dependent drugs. The key factor is whether the duodenum (the first part of the small intestine) is still part of the food path. If it’s bypassed, absorption drops significantly.
Can I still take my extended-release pills after surgery?
It’s risky. Extended-release pills are designed to release slowly over hours. After surgery, especially RYGB, food and pills move through the gut too quickly for these formulations to work. Studies show 40-60% of these drugs lose effectiveness. The American Society for Metabolic and Bariatric Surgery recommends switching to immediate-release versions whenever possible. For example, switch metformin ER to regular metformin taken twice daily.
Why does my thyroid medication need a higher dose after surgery?
Levothyroxine is absorbed in the upper small intestine. After gastric bypass, that area is bypassed, and stomach acid levels rise, reducing the drug’s ability to dissolve properly. Studies show a 25-30% drop in bioavailability. Many patients need a 20-50% increase in dose. Always check your TSH levels 4-6 weeks after surgery and adjust based on lab results, not how you feel.
Should I take my meds with food or on an empty stomach?
It depends on the drug. Acid-dependent medications like levothyroxine, atazanavir, and ketoconazole work best on an empty stomach-30 to 60 minutes before eating. Fat-soluble drugs like griseofulvin or some vitamins need food to absorb properly. Extended-release drugs often work better without food to avoid rapid transit. Always check with your pharmacist or prescriber for your specific meds.
How often should I get blood tests after bariatric surgery?
For high-risk drugs like warfarin, phenytoin, cyclosporine, and lithium, check levels 4-6 weeks after surgery, then every 3 months. For thyroid meds (levothyroxine), check TSH at 6 weeks and then every 6 months. Calcium and vitamin D levels should be checked every 6-12 months. If you’re on any medication with a narrow therapeutic window, regular monitoring isn’t optional-it’s essential.


Comments
Post Comment